Sunday Poster Session
Category: Small Intestine
P1295 - A Case of Bouveret’s Syndrome Resulting in Severe Proximal Small Bowel Obstruction
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- JW
Jade Wang, MD
Weill Cornell Medicine
New York, NY
Presenting Author(s)
Jade Wang, MD1, Vladislav Fomin, MD2, David Wan, BS, MD1
1Weill Cornell Medicine, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medical College, New York, NY
Introduction: Bouveret’s syndrome is a rare form of gallstone ileus characterized by gastric outlet obstruction due to an impacted gallstone that has migrated through a spontaneous cholecystoduodenal fistula. Endoscopic or surgical stone removal are the most common treatment approaches.
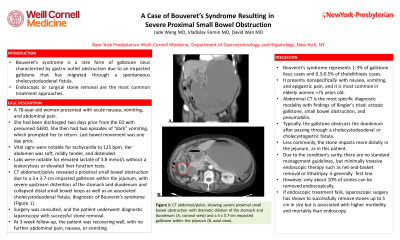
Case Description/Methods: A 78-year-old woman with a history of coronary artery disease and hypertension presented with acute nausea, vomiting, and abdominal pain. She had been discharged two days prior from the ED with presumed GERD after a negative cardiac workup for intermittent chest pain and globus sensation. She then had two episodes of “dark” vomiting, which prompted her to return. Her last bowel movement was one day prior. Vital signs were notable for tachycardia to 125 bpm. Her abdomen was soft, mildly tender, and distended. Labs were notable for elevated lactate of 3.8 mmol/L without a leukocytosis or elevated liver function tests. CT abdomen/pelvis revealed a proximal small bowel obstruction due to a 3 x 3.7-cm impacted gallstone within the jejunum, with severe upstream distention of the stomach and duodenum and collapsed distal small bowel loops as well as an associated cholecystoduodenal fistula, diagnostic of Bouveret’s syndrome (Figure 1). Surgery was consulted, and the patient underwent diagnostic laparoscopy with successful stone removal. At 3-week follow-up, the patient was recovering well, with no further abdominal pain, nausea, or vomiting.
Discussion: Bouveret’s syndrome represents 1-3% of gallstone ileus cases and 0.3-0.5% of cholelithiasis cases. It presents nonspecifically with nausea, vomiting, and epigastric pain, and it is most common in elderly women > 75 years old. Abdominal CT is the most specific diagnostic modality with findings of Ringler’s triad: ectopic gallstone, small bowel obstruction, and pneumobilia. Typically, the gallstone obstructs the duodenum after passing through a cholecystoduodenal or cholecystogastric fistula. Less commonly, the stone impacts more distally in the jejunum, as in this patient. Due to the condition’s rarity, there are no standard management guidelines, but minimally invasive endoscopic therapy such as net-and-basket removal or lithotripsy is generally considered first line. However, only about 10% of stones can be removed endoscopically. If endoscopic treatment fails, laparoscopic surgery has shown to successfully remove stones up to 5 cm in size but is associated with higher morbidity and mortality than endoscopy.

Disclosures:
Jade Wang, MD1, Vladislav Fomin, MD2, David Wan, BS, MD1. P1295 - A Case of Bouveret’s Syndrome Resulting in Severe Proximal Small Bowel Obstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Weill Cornell Medicine, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medical College, New York, NY
Introduction: Bouveret’s syndrome is a rare form of gallstone ileus characterized by gastric outlet obstruction due to an impacted gallstone that has migrated through a spontaneous cholecystoduodenal fistula. Endoscopic or surgical stone removal are the most common treatment approaches.
Case Description/Methods: A 78-year-old woman with a history of coronary artery disease and hypertension presented with acute nausea, vomiting, and abdominal pain. She had been discharged two days prior from the ED with presumed GERD after a negative cardiac workup for intermittent chest pain and globus sensation. She then had two episodes of “dark” vomiting, which prompted her to return. Her last bowel movement was one day prior. Vital signs were notable for tachycardia to 125 bpm. Her abdomen was soft, mildly tender, and distended. Labs were notable for elevated lactate of 3.8 mmol/L without a leukocytosis or elevated liver function tests. CT abdomen/pelvis revealed a proximal small bowel obstruction due to a 3 x 3.7-cm impacted gallstone within the jejunum, with severe upstream distention of the stomach and duodenum and collapsed distal small bowel loops as well as an associated cholecystoduodenal fistula, diagnostic of Bouveret’s syndrome (Figure 1). Surgery was consulted, and the patient underwent diagnostic laparoscopy with successful stone removal. At 3-week follow-up, the patient was recovering well, with no further abdominal pain, nausea, or vomiting.
Discussion: Bouveret’s syndrome represents 1-3% of gallstone ileus cases and 0.3-0.5% of cholelithiasis cases. It presents nonspecifically with nausea, vomiting, and epigastric pain, and it is most common in elderly women > 75 years old. Abdominal CT is the most specific diagnostic modality with findings of Ringler’s triad: ectopic gallstone, small bowel obstruction, and pneumobilia. Typically, the gallstone obstructs the duodenum after passing through a cholecystoduodenal or cholecystogastric fistula. Less commonly, the stone impacts more distally in the jejunum, as in this patient. Due to the condition’s rarity, there are no standard management guidelines, but minimally invasive endoscopic therapy such as net-and-basket removal or lithotripsy is generally considered first line. However, only about 10% of stones can be removed endoscopically. If endoscopic treatment fails, laparoscopic surgery has shown to successfully remove stones up to 5 cm in size but is associated with higher morbidity and mortality than endoscopy.

Figure: Figure 1: CT abdomen/pelvis showing severe proximal small bowel obstruction with dramatic dilation of the stomach and duodenum (A, coronal view) and a 3 x 3.7-cm impacted gallstone within the jejunum (B, axial view).
Disclosures:
Jade Wang indicated no relevant financial relationships.
Vladislav Fomin indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Jade Wang, MD1, Vladislav Fomin, MD2, David Wan, BS, MD1. P1295 - A Case of Bouveret’s Syndrome Resulting in Severe Proximal Small Bowel Obstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
