Sunday Poster Session
Category: Small Intestine
P1300 - An Atypical Presentation of Collagenous Gastroenteritides
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Mazen Almasry, MBBS
University of Wisconsin-Madison School of Medicine and Public Health
Madison, WI
Presenting Author(s)
Mazen Almasry, MBBS1, Hashem Al Bunni, MBBS2, Saqib Walayat, MBBS1, Anurag Soni, MBBS1, Mark Benson, MD3
1University of Wisconsin-Madison School of Medicine and Public Health, Madison, WI; 2IU Health University Hospital, Indianapolis, IN; 3University of Wisconsin School of Medicine, Madison, WI
Introduction: Collagenous gastroenteritides (CG) are characterized by a subepithelial collagen deposition with entrapped inflammatory cells and capillaries, forming a band with a width of more than 10 µm. CG most commonly affect the colon (collagenous colitis), infrequently the small intestine (collagenous sprue, 120 cases reported), and rarely the stomach (collagenous gastritis, 168 cases reported). Typically, patients with CG present with diarrhea, weight loss, and malabsorption. Various therapy strategies have been published in case studies; however, there is not a consensus on the best treatment strategy. Herein, we present a case of concurrent collagenous sprue and collagenous gastritis with atypical presentation.
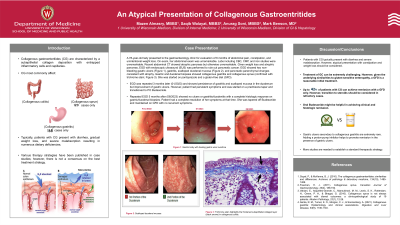
Case Description/Methods: A 78-year-old lady presented to GI clinic for evaluation of abdominal pain, nausea, constipation and unintentional weight loss. Symptoms have been intermittent for 6 months. On physical examination, her abdomen was soft and non-tender with normal bowel sounds. Labs including CBC, comprehensive metabolic panel and iron studies were unremarkable. Recent abdominal CTA showed atrophic pancreas and atherosclerotic changes of the proximal celiac artery with the distal segment remaining opacified. Given weight loss and atrophic pancreas, EGD with EUS was performed to rule out pancreatic cancer. EGD showed two non-bleeding gastric ulcers, gastritis, scalloped duodenal mucosa and pancreatic parenchymal changes consistent with atrophy. Gastric and duodenal biopsies showed collagenous gastritis and collagenous sprue, respectively. She was started on PPI and a gluten-free diet (GFD). EGD was repeated 3 months later and showed persistence of gastritis and scalloped mucosa in the duodenum but improvement of gastric ulcers. She was started on a prednisone taper and transitioned to Budesonide. She had a complete resolution of her symptoms after.
Discussion: Patients with CG typically present with diarrhea and malabsorption. However, atypical presentation with constipation and weight loss should be considered. In addition, gastric ulcers secondary to collagenous gastritis are extremely rare. Treatment of GC can be extremely challenging as there is not universal treatment strategy. Given similarities to gluten-sensitive enteropathy, a GFD is a reasonable initial treatment. Up to 42% of patients with CG can achieve remission with a GFD only. However, transition to steroids should be considered in refractory cases. Adding a PPI helps to promote remission in the presence of gastric ulcers.

Disclosures:
Mazen Almasry, MBBS1, Hashem Al Bunni, MBBS2, Saqib Walayat, MBBS1, Anurag Soni, MBBS1, Mark Benson, MD3. P1300 - An Atypical Presentation of Collagenous Gastroenteritides, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Wisconsin-Madison School of Medicine and Public Health, Madison, WI; 2IU Health University Hospital, Indianapolis, IN; 3University of Wisconsin School of Medicine, Madison, WI
Introduction: Collagenous gastroenteritides (CG) are characterized by a subepithelial collagen deposition with entrapped inflammatory cells and capillaries, forming a band with a width of more than 10 µm. CG most commonly affect the colon (collagenous colitis), infrequently the small intestine (collagenous sprue, 120 cases reported), and rarely the stomach (collagenous gastritis, 168 cases reported). Typically, patients with CG present with diarrhea, weight loss, and malabsorption. Various therapy strategies have been published in case studies; however, there is not a consensus on the best treatment strategy. Herein, we present a case of concurrent collagenous sprue and collagenous gastritis with atypical presentation.
Case Description/Methods: A 78-year-old lady presented to GI clinic for evaluation of abdominal pain, nausea, constipation and unintentional weight loss. Symptoms have been intermittent for 6 months. On physical examination, her abdomen was soft and non-tender with normal bowel sounds. Labs including CBC, comprehensive metabolic panel and iron studies were unremarkable. Recent abdominal CTA showed atrophic pancreas and atherosclerotic changes of the proximal celiac artery with the distal segment remaining opacified. Given weight loss and atrophic pancreas, EGD with EUS was performed to rule out pancreatic cancer. EGD showed two non-bleeding gastric ulcers, gastritis, scalloped duodenal mucosa and pancreatic parenchymal changes consistent with atrophy. Gastric and duodenal biopsies showed collagenous gastritis and collagenous sprue, respectively. She was started on PPI and a gluten-free diet (GFD). EGD was repeated 3 months later and showed persistence of gastritis and scalloped mucosa in the duodenum but improvement of gastric ulcers. She was started on a prednisone taper and transitioned to Budesonide. She had a complete resolution of her symptoms after.
Discussion: Patients with CG typically present with diarrhea and malabsorption. However, atypical presentation with constipation and weight loss should be considered. In addition, gastric ulcers secondary to collagenous gastritis are extremely rare. Treatment of GC can be extremely challenging as there is not universal treatment strategy. Given similarities to gluten-sensitive enteropathy, a GFD is a reasonable initial treatment. Up to 42% of patients with CG can achieve remission with a GFD only. However, transition to steroids should be considered in refractory cases. Adding a PPI helps to promote remission in the presence of gastric ulcers.

Figure: 2nd Portion of the Duedenum
Disclosures:
Mazen Almasry indicated no relevant financial relationships.
Hashem Al Bunni indicated no relevant financial relationships.
Saqib Walayat indicated no relevant financial relationships.
Anurag Soni indicated no relevant financial relationships.
Mark Benson indicated no relevant financial relationships.
Mazen Almasry, MBBS1, Hashem Al Bunni, MBBS2, Saqib Walayat, MBBS1, Anurag Soni, MBBS1, Mark Benson, MD3. P1300 - An Atypical Presentation of Collagenous Gastroenteritides, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

