Sunday Poster Session
Category: Small Intestine
P1309 - A Rare Case of Pure Choriocarcinoma Metastasis to the Duodenum in a Male With Previous Mixed Germ Cell Tumor
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Parvir Aujla, MD
University of Texas Health Science Center
Houston, TX
Presenting Author(s)
Parvir Aujla, MD1, Rohit Khanna, DO2, Abdullah Aleem, MD3, John Lyons, MD2
1University of Texas Health Science Center, Houston, TX; 2Scripps Clinic, La Jolla, CA; 3University of Texas Health Science Center, Houston, AZ
Introduction: Pure Choriocarcinoma (PCC), an aggressive subtype of germ cell tumors, rarely metastasizes to the gastrointestinal (GI) tract, and a paucity of case reports describe GI bleed as the presenting symptom. A patient with a history of mixed germ cell tumor in remission presented with new-onset melena. Endoscopy revealed a bleeding, ulcerated duodenal mass and liver biopsy confirmed a new diagnosis of metastatic PCC.
Case Description/Methods: A 52 year old male with a history of mixed-germ cell testicular cancer (1999) status post right sided orchiectomy with recurrence resulting in retroperitoneal lymph node dissection and autologous stem cell transplant (2003) in remission presented with new-onset black tarry stools and solid-food dysphagia. He denied nausea, vomiting, diarrhea, unintentional weight loss, fevers, night sweats, sick contacts. He reported increased NSAID intake for one week for a right hand injury. Colonoscopy 8-months prior revealed sessile serrated and tubular adenomatous polyps. Social history includes a 20-pack year history and previous alcohol use disorder. Oncology work-up two years prior to admission demonstrated negative CT abdomen and pelvis and an undetectable AFP.
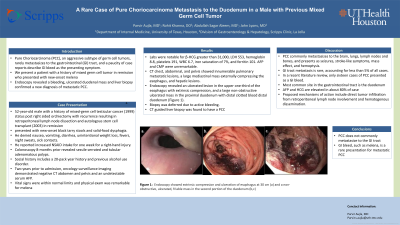
Physical exam was significant for melena. Labs notable for β-HCG >31,000, LDH 553, Hbg 8.8, PLT 191, WBC 6.7, iron sat 7, and ferritin 101. AFP and CMP were unremarkable. CT chest, abdominal, and pelvis showed innumerable pulmonary metastatic lesion, a large mediastinal mass externally compressing the esophagus,and hepatic lesions. Endoscopy revealed an ulcerated lesion in the upper one-third of the esophagus with extrinsic compression, and a large non-obstructive ulcerated mass in the proximal duodenum with distal clotted blood distal duodenum (Figure 1). Biopsy was deferred due to active bleeding. CT guided liver biopsy was found to have a PCC. Patient was referred to oncology for staging and treatment.
Discussion: PCC commonly metastasizes to the brain, lungs, lymph nodes and bones, and presents as seizures, stroke-like symptoms, mass effect, and hemoptysis. GI tract metastasis is rare, accounting for less than 5% of all cases. In a recent literature review, only sixteen cases of PCC presented as a GI bleed. Proposed mechanisms of action include direct tumor infiltration from retroperitoneal lymph node involvement and hematogenous dissemination. New-onset melena is a rare presentation for PCC and should be considered in the differential.

Disclosures:
Parvir Aujla, MD1, Rohit Khanna, DO2, Abdullah Aleem, MD3, John Lyons, MD2. P1309 - A Rare Case of Pure Choriocarcinoma Metastasis to the Duodenum in a Male With Previous Mixed Germ Cell Tumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Health Science Center, Houston, TX; 2Scripps Clinic, La Jolla, CA; 3University of Texas Health Science Center, Houston, AZ
Introduction: Pure Choriocarcinoma (PCC), an aggressive subtype of germ cell tumors, rarely metastasizes to the gastrointestinal (GI) tract, and a paucity of case reports describe GI bleed as the presenting symptom. A patient with a history of mixed germ cell tumor in remission presented with new-onset melena. Endoscopy revealed a bleeding, ulcerated duodenal mass and liver biopsy confirmed a new diagnosis of metastatic PCC.
Case Description/Methods: A 52 year old male with a history of mixed-germ cell testicular cancer (1999) status post right sided orchiectomy with recurrence resulting in retroperitoneal lymph node dissection and autologous stem cell transplant (2003) in remission presented with new-onset black tarry stools and solid-food dysphagia. He denied nausea, vomiting, diarrhea, unintentional weight loss, fevers, night sweats, sick contacts. He reported increased NSAID intake for one week for a right hand injury. Colonoscopy 8-months prior revealed sessile serrated and tubular adenomatous polyps. Social history includes a 20-pack year history and previous alcohol use disorder. Oncology work-up two years prior to admission demonstrated negative CT abdomen and pelvis and an undetectable AFP.
Physical exam was significant for melena. Labs notable for β-HCG >31,000, LDH 553, Hbg 8.8, PLT 191, WBC 6.7, iron sat 7, and ferritin 101. AFP and CMP were unremarkable. CT chest, abdominal, and pelvis showed innumerable pulmonary metastatic lesion, a large mediastinal mass externally compressing the esophagus,and hepatic lesions. Endoscopy revealed an ulcerated lesion in the upper one-third of the esophagus with extrinsic compression, and a large non-obstructive ulcerated mass in the proximal duodenum with distal clotted blood distal duodenum (Figure 1). Biopsy was deferred due to active bleeding. CT guided liver biopsy was found to have a PCC. Patient was referred to oncology for staging and treatment.
Discussion: PCC commonly metastasizes to the brain, lungs, lymph nodes and bones, and presents as seizures, stroke-like symptoms, mass effect, and hemoptysis. GI tract metastasis is rare, accounting for less than 5% of all cases. In a recent literature review, only sixteen cases of PCC presented as a GI bleed. Proposed mechanisms of action include direct tumor infiltration from retroperitoneal lymph node involvement and hematogenous dissemination. New-onset melena is a rare presentation for PCC and should be considered in the differential.

Figure: Figure 1: Endoscopy showed extrinsic compression and ulceration of esophagus at 30 cm (a) and a non-obstructive, ulcerated, friable mass in the second portion of the duodenum (b,c).
Disclosures:
Parvir Aujla indicated no relevant financial relationships.
Rohit Khanna indicated no relevant financial relationships.
Abdullah Aleem indicated no relevant financial relationships.
John Lyons indicated no relevant financial relationships.
Parvir Aujla, MD1, Rohit Khanna, DO2, Abdullah Aleem, MD3, John Lyons, MD2. P1309 - A Rare Case of Pure Choriocarcinoma Metastasis to the Duodenum in a Male With Previous Mixed Germ Cell Tumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
