Sunday Poster Session
Category: Small Intestine
P1329 - Duodenal Adenocarcinoma and Celiac Disease: Association or Coincidence?
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Danial Nadeem, MD
Geisinger Medical Center
Bloomsburg, PA
Presenting Author(s)
Danial Nadeem, MD1, David L. Diehl, MD1, Hongjie Li, MD, PhD2
1Geisinger Medical Center, Danville, PA; 2Geisinger, Danville, PA
Introduction: While there are known associations between Celiac Disease (CD) and lymphoma, the association between CD and small bowel adenocarcinoma (SBA) is not as clear.1 Herein we present the case of a patient with CD who presented with duodenal obstruction and was found to have a signet cell duodenal adenocarcinoma.
Case Description/Methods: A 62-year-old man with a longstanding history of CD presented with worsening abdominal pain, nausea and vomiting associated with an 18-pound weight loss over the preceding two months. Contrast-enhanced computed tomography (CT) and follow up esophagogastroduodenoscopy (EGD) with endoscopic ultrasound (EUS) confirmed a large fungating mass in the second portion of the duodenum. Fine needle biopsy was performed and pathology of the resected tissue showed poorly differentiated signet ring cell adenocarcinoma.
Four weeks later, pancreaticoduodenectomy was performed without complication. The patient was referred to radiation oncology to begin treatment with radiation and chemotherapy.
Discussion: CD has a known association with many types of lymphomas, but is less known to be associated with malignancies such as SBA.1,2 Current estimates report a 60- to 80-fold increased risk of SBA in CD patients with low adherence to a gluten free diet.3 Signet cell SBA is a special subtype of adenocarcinoma with a generally worse prognosis, whose appearance is most often associated with malignancy.4
Risk factors for the development of SBA in CD patients include smoking history, alcohol use, as well as a longer duration of CD, leading to malabsorption of anticarcinogenic vitamins.3,5 Treatment for signet cell SBA usually includes surgical resection, accompanied by adjuvant radiation or chemotherapy. Due to the rarity of signet cell SBA, comprehensive data regarding causes and treatment is lacking.
Patients with CD are up to 80 times more likely to develop SBA than the general population.6 This case highlights the importance of considering SBA as a potential complication of CD, particularly in patients with unexplained weight loss, abdominal pain, and obstructive symptoms. Despite the rarity of this malignancy, one should maintain a high index of suspicion and conduct prompt diagnostic workup to improve patient outcomes.

Disclosures:
Danial Nadeem, MD1, David L. Diehl, MD1, Hongjie Li, MD, PhD2. P1329 - Duodenal Adenocarcinoma and Celiac Disease: Association or Coincidence?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Geisinger Medical Center, Danville, PA; 2Geisinger, Danville, PA
Introduction: While there are known associations between Celiac Disease (CD) and lymphoma, the association between CD and small bowel adenocarcinoma (SBA) is not as clear.1 Herein we present the case of a patient with CD who presented with duodenal obstruction and was found to have a signet cell duodenal adenocarcinoma.
Case Description/Methods: A 62-year-old man with a longstanding history of CD presented with worsening abdominal pain, nausea and vomiting associated with an 18-pound weight loss over the preceding two months. Contrast-enhanced computed tomography (CT) and follow up esophagogastroduodenoscopy (EGD) with endoscopic ultrasound (EUS) confirmed a large fungating mass in the second portion of the duodenum. Fine needle biopsy was performed and pathology of the resected tissue showed poorly differentiated signet ring cell adenocarcinoma.
Four weeks later, pancreaticoduodenectomy was performed without complication. The patient was referred to radiation oncology to begin treatment with radiation and chemotherapy.
Discussion: CD has a known association with many types of lymphomas, but is less known to be associated with malignancies such as SBA.1,2 Current estimates report a 60- to 80-fold increased risk of SBA in CD patients with low adherence to a gluten free diet.3 Signet cell SBA is a special subtype of adenocarcinoma with a generally worse prognosis, whose appearance is most often associated with malignancy.4
Risk factors for the development of SBA in CD patients include smoking history, alcohol use, as well as a longer duration of CD, leading to malabsorption of anticarcinogenic vitamins.3,5 Treatment for signet cell SBA usually includes surgical resection, accompanied by adjuvant radiation or chemotherapy. Due to the rarity of signet cell SBA, comprehensive data regarding causes and treatment is lacking.
Patients with CD are up to 80 times more likely to develop SBA than the general population.6 This case highlights the importance of considering SBA as a potential complication of CD, particularly in patients with unexplained weight loss, abdominal pain, and obstructive symptoms. Despite the rarity of this malignancy, one should maintain a high index of suspicion and conduct prompt diagnostic workup to improve patient outcomes.

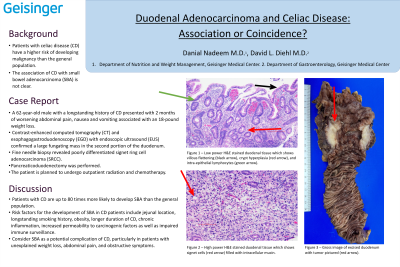
Figure: Figure 1 – Gross image of excised duodenum with tumor.
Figure 2 – Low power H&E stained duodenal tissue showing villous flattening (black arrow), crypt hyperplasia (yellow arrow) as well as increased intra-epithelial lymphocytes (green arrow), indicative of Celiac disease.
Figure 3 – High power H&E stained duodenal tissue showing signet cells (red arrow) filled with intracellular mucin.
Figure 2 – Low power H&E stained duodenal tissue showing villous flattening (black arrow), crypt hyperplasia (yellow arrow) as well as increased intra-epithelial lymphocytes (green arrow), indicative of Celiac disease.
Figure 3 – High power H&E stained duodenal tissue showing signet cells (red arrow) filled with intracellular mucin.
Disclosures:
Danial Nadeem indicated no relevant financial relationships.
David Diehl: Boston Scientific – Consultant. Castle – Consultant. Laborie – Consultant. Merit Endotek – Consultant. Microtech – Consultant. Olympus – Consultant. OnePass Medical – Consultant. Pentax – Consultant. Steris – Consultant.
Hongjie Li indicated no relevant financial relationships.
Danial Nadeem, MD1, David L. Diehl, MD1, Hongjie Li, MD, PhD2. P1329 - Duodenal Adenocarcinoma and Celiac Disease: Association or Coincidence?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
