Sunday Poster Session
Category: Stomach
P1361 - A Unique Case of Pyloric Gastric Adenoma: Endoscopic Detection, Echoendosonographic Characterization, and Removal
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- AL
Anabel Liyen Cartelle, MD
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Presenting Author(s)
Anabel Liyen Cartelle, MD1, Erik Holzwanger, MD1, Samuel Igbinedion, MD2, Sultan Mahmood, MD1, Harry Rosenberg, MD1, Tyler Berzin, MD, FACG1, Mandeep Sawhney, MD, MS1, Moamen Gabr, MD, MSc,1, Douglas Pleskow, MD, FACG3
1Beth Israel Deaconess Medical Center, Boston, MA; 2Center for Advanced Endoscopy, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 3BIDMC, Boston, MA
Introduction: Pyloric gland adenomas (PGA) are rare precancerous epithelial polyps that exhibit gastric pyloric gland differentiation. Correct diagnosis is important given high malignant potential. We present a unique case of a female patient with gastroesophageal reflux disease (GERD) found to have a suspected subepithelial lesion (SEL), characterized by echoendosonography (EUS), with histopathologic identification as a PGA.
Case Description/Methods: A 62-year-old woman with a past medical history of rheumatoid arthritis, anemia, and GERD presented as a referral for EUS after she was found to have a 10 mm subepithelial nodule within a hiatal hernia on a previous EGD. She had an unremarkable physical exam, vital signs, and laboratory studies. Her upper endoscopy revealed a small hiatal hernia and distal grade A esophagitis. In the stomach, diffuse erythema was compatible with gastropathy. A single sessile 10mm polyp was detected within the hiatal hernia sac. EUS was then performed which revealed a thickened mucosal layer in the distal esophagus, however no discrete lesions. The polyp was removed via a single piece hot snare polypectomy. Histologically, glandular proliferation of back-to-back mucinous glands was present, consistent with a pyloric gland adenoma with no signs of dysplasia. She was advised to return in 6 months for surveillance endoscopy.
Discussion: We present the case of a PGA found within a hiatal hernia sac. These neoplasms are challenging to diagnose, and surveillance has not been standardized due to their rarity. PGAs account for 2-2.7% of all gastric adenomas, with reported advancement to adenocarcinoma in 12-47% of cases. Grossly, PGAs can appear as polypoid lesions, although some can be irregular mucosal, flat, ulcerative, or even submucosal tumor-like. Histologically, they are characterized by back-to-back pyloric glands that are well-demarcated from the surrounding mucosa. Wide acceptance of PGAs as an entity in North America was delayed until 2009 with the publication of the second largest case series in the literature at the time by Chen et al. from Johns Hopkins. This case series corroborated previously noted female predominance, location in the gastric body, and association with autoimmune gastritis. As with our case, EUS can assist in evaluation and locoregional staging of these lesions. Increased recognition by endoscopists is paramount and further endoscopic surveillance guidelines are needed to minimize future malignant transformation.

Disclosures:
Anabel Liyen Cartelle, MD1, Erik Holzwanger, MD1, Samuel Igbinedion, MD2, Sultan Mahmood, MD1, Harry Rosenberg, MD1, Tyler Berzin, MD, FACG1, Mandeep Sawhney, MD, MS1, Moamen Gabr, MD, MSc,1, Douglas Pleskow, MD, FACG3. P1361 - A Unique Case of Pyloric Gastric Adenoma: Endoscopic Detection, Echoendosonographic Characterization, and Removal, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Boston, MA; 2Center for Advanced Endoscopy, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 3BIDMC, Boston, MA
Introduction: Pyloric gland adenomas (PGA) are rare precancerous epithelial polyps that exhibit gastric pyloric gland differentiation. Correct diagnosis is important given high malignant potential. We present a unique case of a female patient with gastroesophageal reflux disease (GERD) found to have a suspected subepithelial lesion (SEL), characterized by echoendosonography (EUS), with histopathologic identification as a PGA.
Case Description/Methods: A 62-year-old woman with a past medical history of rheumatoid arthritis, anemia, and GERD presented as a referral for EUS after she was found to have a 10 mm subepithelial nodule within a hiatal hernia on a previous EGD. She had an unremarkable physical exam, vital signs, and laboratory studies. Her upper endoscopy revealed a small hiatal hernia and distal grade A esophagitis. In the stomach, diffuse erythema was compatible with gastropathy. A single sessile 10mm polyp was detected within the hiatal hernia sac. EUS was then performed which revealed a thickened mucosal layer in the distal esophagus, however no discrete lesions. The polyp was removed via a single piece hot snare polypectomy. Histologically, glandular proliferation of back-to-back mucinous glands was present, consistent with a pyloric gland adenoma with no signs of dysplasia. She was advised to return in 6 months for surveillance endoscopy.
Discussion: We present the case of a PGA found within a hiatal hernia sac. These neoplasms are challenging to diagnose, and surveillance has not been standardized due to their rarity. PGAs account for 2-2.7% of all gastric adenomas, with reported advancement to adenocarcinoma in 12-47% of cases. Grossly, PGAs can appear as polypoid lesions, although some can be irregular mucosal, flat, ulcerative, or even submucosal tumor-like. Histologically, they are characterized by back-to-back pyloric glands that are well-demarcated from the surrounding mucosa. Wide acceptance of PGAs as an entity in North America was delayed until 2009 with the publication of the second largest case series in the literature at the time by Chen et al. from Johns Hopkins. This case series corroborated previously noted female predominance, location in the gastric body, and association with autoimmune gastritis. As with our case, EUS can assist in evaluation and locoregional staging of these lesions. Increased recognition by endoscopists is paramount and further endoscopic surveillance guidelines are needed to minimize future malignant transformation.

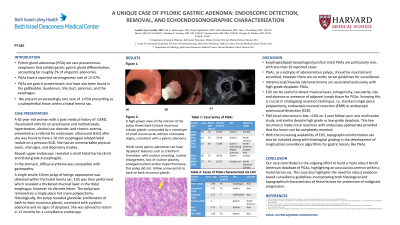
Figure: Upper endoscopy of the upper esophagus. (A)Yellow arrow points at lesion located within the hiatal hernia distal to the GE junction. (B) Endoscopic ultrasound (radial 5-7 Hz) image taken at region of the polyp prior to excision reveals a thickened esophageal wall but no clear mucosal/submucosal lesion. (C) A low-power view of the polyp shows a polypoid fragment of stomach mucosal epithelium with glandular proliferation. (D) A high-power view shows back-to-back mucinous glands (yellow arrow), consistent with a pyloric adenoma. While many pyloric adenomas can have dysplasia, this polyp did not.
Disclosures:
Anabel Liyen Cartelle indicated no relevant financial relationships.
Erik Holzwanger indicated no relevant financial relationships.
Samuel Igbinedion indicated no relevant financial relationships.
Sultan Mahmood indicated no relevant financial relationships.
Harry Rosenberg indicated no relevant financial relationships.
Tyler Berzin: Boston Scientific – Consultant. Fuji – Consultant. Medtronic – Consultant.
Mandeep Sawhney: Allurion – Stock Options. Immunovia Inc. – Consultant. Marlborough, MA – Consultant.
Moamen Gabr: Adaptive Endo – Consultant. Boston Scientific – Consultant. ConMed – Consultant. Fuji – Consultant. Medtronic – Consultant. Olympus – Consultant.
Douglas Pleskow: Boston Scientific – Consultant. Fuji – Consultant. Olympus – Consultant.
Anabel Liyen Cartelle, MD1, Erik Holzwanger, MD1, Samuel Igbinedion, MD2, Sultan Mahmood, MD1, Harry Rosenberg, MD1, Tyler Berzin, MD, FACG1, Mandeep Sawhney, MD, MS1, Moamen Gabr, MD, MSc,1, Douglas Pleskow, MD, FACG3. P1361 - A Unique Case of Pyloric Gastric Adenoma: Endoscopic Detection, Echoendosonographic Characterization, and Removal, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
