Sunday Poster Session
Category: Stomach
P1365 - Severe Anemia as Initial Presentation of Hepatic Abscess Secondary to Subclinical Gastric Ulcer Perforation
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- TG
Tyler Grantham, MD
Staten Island University Hospital
Staten Island, NY
Presenting Author(s)
Rajarajeshwari Ramachandran, MD1, Tyler Grantham, MD2, Vikash Kumar, MD1, Denzil Etienne, MD1, Vinaya Gaduputi, MD3
1Brooklyn Hospital Center, Brooklyn, NY; 2Staten Island University Hospital, Staten Island, NY; 3Blanchard Valley Health System, Findlay, OH
Introduction: Peptic ulcer disease (PUD) remains a significant healthcare burden despite widespread use of proton pump inhibitors. In the United States, bleeding is the most common complication of PUD, followed by perforation. We are reporting a case of hepatic and intra-abdominal abscesses secondary to subclinical gastric ulcer perforation.
Case Description/Methods: A 28-year-old woman was diagnosed with severe anemia of unknown etiology during workup of severe fatigue. She suffered from arthralgias and was using ibuprofen 800 mg three times a day for several months. She had mild, diffuse abdominal tenderness, without guarding, rebound, rigidity or signs of overt gastrointestinal bleeding.
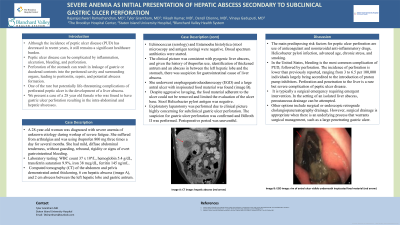
Laboratory testing: WBC count 37 x 10⁹/L, hemoglobin 5.4 g/dL, transferrin saturation 9.9%, iron 38 mcg/dL, ferritin 145 ng/mL. Computed tomography (CT) of the abdomen and pelvis demonstrated antral thickening, 6 cm hepatic abscess (image A), and 2 cm abscess between the left hepatic lobe and gastric antrum. Testing for Echinococcus (serology) and Entamoeba histolytica (stool microscopy and antigen testing) were negative. Broad spectrum antibiotics were started.
The clinical picture was consistent with pyogenic liver abscess, and given the history of ibuprofen use, identification of thickened antrum and an abscess in between the left hepatic lobe and the stomach, there was suspicion for gastrointestinal cause of liver abscess. She underwent esophagogastroduodenoscopy (EGD) and a large antral ulcer with inspissated food material was found (image B). Despite aggressive lavaging, the food material adherent to the ulcer could not be removed and limited the evaluation of the ulcer base. Stool Helicobacter pylori antigen was negative.
Exploratory laparotomy was performed due to clinical picture highly concerning for subclinical gastric ulcer perforation. The suspicion for gastric ulcer perforation was confirmed and Billroth II was performed. Postoperative period was uneventful.
Discussion: Predisposing factors for gastric ulcer perforation are Helicobacter pylori infection, advanced age, smoking, use of anticoagulants or nonsteroidal anti-inflammatory drugs. Ulcer perforation resulting in liver abscess is a rare complication of PUD. Our patient presented symptomatic anemia and was diagnosed with hepatic and intra-abdominal abscesses secondary to subclinical gastric ulcer perforation. She was successfully treated with antibiotics and surgery.

Disclosures:
Rajarajeshwari Ramachandran, MD1, Tyler Grantham, MD2, Vikash Kumar, MD1, Denzil Etienne, MD1, Vinaya Gaduputi, MD3. P1365 - Severe Anemia as Initial Presentation of Hepatic Abscess Secondary to Subclinical Gastric Ulcer Perforation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brooklyn Hospital Center, Brooklyn, NY; 2Staten Island University Hospital, Staten Island, NY; 3Blanchard Valley Health System, Findlay, OH
Introduction: Peptic ulcer disease (PUD) remains a significant healthcare burden despite widespread use of proton pump inhibitors. In the United States, bleeding is the most common complication of PUD, followed by perforation. We are reporting a case of hepatic and intra-abdominal abscesses secondary to subclinical gastric ulcer perforation.
Case Description/Methods: A 28-year-old woman was diagnosed with severe anemia of unknown etiology during workup of severe fatigue. She suffered from arthralgias and was using ibuprofen 800 mg three times a day for several months. She had mild, diffuse abdominal tenderness, without guarding, rebound, rigidity or signs of overt gastrointestinal bleeding.
Laboratory testing: WBC count 37 x 10⁹/L, hemoglobin 5.4 g/dL, transferrin saturation 9.9%, iron 38 mcg/dL, ferritin 145 ng/mL. Computed tomography (CT) of the abdomen and pelvis demonstrated antral thickening, 6 cm hepatic abscess (image A), and 2 cm abscess between the left hepatic lobe and gastric antrum. Testing for Echinococcus (serology) and Entamoeba histolytica (stool microscopy and antigen testing) were negative. Broad spectrum antibiotics were started.
The clinical picture was consistent with pyogenic liver abscess, and given the history of ibuprofen use, identification of thickened antrum and an abscess in between the left hepatic lobe and the stomach, there was suspicion for gastrointestinal cause of liver abscess. She underwent esophagogastroduodenoscopy (EGD) and a large antral ulcer with inspissated food material was found (image B). Despite aggressive lavaging, the food material adherent to the ulcer could not be removed and limited the evaluation of the ulcer base. Stool Helicobacter pylori antigen was negative.
Exploratory laparotomy was performed due to clinical picture highly concerning for subclinical gastric ulcer perforation. The suspicion for gastric ulcer perforation was confirmed and Billroth II was performed. Postoperative period was uneventful.
Discussion: Predisposing factors for gastric ulcer perforation are Helicobacter pylori infection, advanced age, smoking, use of anticoagulants or nonsteroidal anti-inflammatory drugs. Ulcer perforation resulting in liver abscess is a rare complication of PUD. Our patient presented symptomatic anemia and was diagnosed with hepatic and intra-abdominal abscesses secondary to subclinical gastric ulcer perforation. She was successfully treated with antibiotics and surgery.

Figure: Image A: CT image: hepatic abscess (red arrow)
Image B: EGD image: rim of antral ulcer visible underneath inspissated food material (red arrow)
Image B: EGD image: rim of antral ulcer visible underneath inspissated food material (red arrow)
Disclosures:
Rajarajeshwari Ramachandran indicated no relevant financial relationships.
Tyler Grantham indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Denzil Etienne indicated no relevant financial relationships.
Vinaya Gaduputi indicated no relevant financial relationships.
Rajarajeshwari Ramachandran, MD1, Tyler Grantham, MD2, Vikash Kumar, MD1, Denzil Etienne, MD1, Vinaya Gaduputi, MD3. P1365 - Severe Anemia as Initial Presentation of Hepatic Abscess Secondary to Subclinical Gastric Ulcer Perforation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
