Sunday Poster Session
Category: Stomach
P1381 - Curative Endoscopic Full Thickness Resection for Gastric Adenocarcinoma pT1bNxMx
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Anusha Singhania, MBBS
Swedish Medical Center
Seattle, WA
Presenting Author(s)
Anusha Singhania, MBBS1, Mohit Girotra, MD2, Rajnish Mishra, MD1
1Swedish Medical Center, Seattle, WA; 2Swedish Medical Center, Washington State University Elson S. Floyd School of Medicine, Seattle, WA
Introduction: Gastric high-grade dysplasia (HGD) is a premalignant lesion and warrants en bloc resection, preferably with endoscopic submucosal dissection (ESD). However, since HGD can harbinger a focus of invasive gastric adenocarcinoma (GC), there can often be residual tumor or lymph node metastasis requiring additional therapies like re-ESD, gastrectomy, wedge resection or ablation.
We report a case of gastric HGD with T1b GC wherein full thickness resection (FTR) was curative.
Case Description/Methods: An 80-year-old man with no family history of cancer or IBD, was discovered to have an endoluminal enlarging gastric body mass (3.4 x 1.9 cm) on CT abdomen, done for persistent post cholecystectomy abdominal pain. Upper endoscopy showed chronic nonerosive gastritis and a fungating, friable, polypoid/semipedunculated 3.5 cm corpus mass with stigmata of recent bleeding and malignant appearance. Biopsy revealed a HGD lesion with surrounding atrophic gastritis, but could not exclude intramucosal GC.
He did not endorse any appetite/weight loss, had no palpable lymph nodes/ abdominal masses and had negative tumor markers.
Endoscopic ultrasound (EUS) staged the lesion as T1N0, for which he underwent ESD/FTR. Histopathology revealed superficially invasive GC arising in a background of gastric adenoma, with high-grade dysplasia pT1b, with no muscularis propria, lymphovascular or perineural invasion; and an adjoining lymph node negative for malignancy. Staging CT after 2 months confirmed complete removal with no recurrence or metastasis, requiring surveillance but no chemotherapy/ radiotherapy.
Discussion: The lower prevalence, leading to paucity of Western data, and variable guidelines, results in inconsistencies in clinical management of early GC, including biopsy proven HGD, which frequently upgrades to GC on endoscopic resection, that has similar efficacy and lower morbidity than gastrectomy.
Based on the EUS-biopsy graded differentiated T1a lesion > 2 cm with ulcer/ scar, our patient fit the expanded criteria for endoscopic resection, which was undertaken using an ESD/FTR hybrid approach, allowing achievement of broader pathologic margins and complete resection of all layers including an adjoining lymph node, which allowed histopathologically and radiologically proven curative resection, obviating the need for further intervention. This is significant considering the local recurrence rates of 4.8-7% for expanded criteria lesions in Western populations, even on short-term follow up.

Disclosures:
Anusha Singhania, MBBS1, Mohit Girotra, MD2, Rajnish Mishra, MD1. P1381 - Curative Endoscopic Full Thickness Resection for Gastric Adenocarcinoma pT1bNxMx, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Swedish Medical Center, Seattle, WA; 2Swedish Medical Center, Washington State University Elson S. Floyd School of Medicine, Seattle, WA
Introduction: Gastric high-grade dysplasia (HGD) is a premalignant lesion and warrants en bloc resection, preferably with endoscopic submucosal dissection (ESD). However, since HGD can harbinger a focus of invasive gastric adenocarcinoma (GC), there can often be residual tumor or lymph node metastasis requiring additional therapies like re-ESD, gastrectomy, wedge resection or ablation.
We report a case of gastric HGD with T1b GC wherein full thickness resection (FTR) was curative.
Case Description/Methods: An 80-year-old man with no family history of cancer or IBD, was discovered to have an endoluminal enlarging gastric body mass (3.4 x 1.9 cm) on CT abdomen, done for persistent post cholecystectomy abdominal pain. Upper endoscopy showed chronic nonerosive gastritis and a fungating, friable, polypoid/semipedunculated 3.5 cm corpus mass with stigmata of recent bleeding and malignant appearance. Biopsy revealed a HGD lesion with surrounding atrophic gastritis, but could not exclude intramucosal GC.
He did not endorse any appetite/weight loss, had no palpable lymph nodes/ abdominal masses and had negative tumor markers.
Endoscopic ultrasound (EUS) staged the lesion as T1N0, for which he underwent ESD/FTR. Histopathology revealed superficially invasive GC arising in a background of gastric adenoma, with high-grade dysplasia pT1b, with no muscularis propria, lymphovascular or perineural invasion; and an adjoining lymph node negative for malignancy. Staging CT after 2 months confirmed complete removal with no recurrence or metastasis, requiring surveillance but no chemotherapy/ radiotherapy.
Discussion: The lower prevalence, leading to paucity of Western data, and variable guidelines, results in inconsistencies in clinical management of early GC, including biopsy proven HGD, which frequently upgrades to GC on endoscopic resection, that has similar efficacy and lower morbidity than gastrectomy.
Based on the EUS-biopsy graded differentiated T1a lesion > 2 cm with ulcer/ scar, our patient fit the expanded criteria for endoscopic resection, which was undertaken using an ESD/FTR hybrid approach, allowing achievement of broader pathologic margins and complete resection of all layers including an adjoining lymph node, which allowed histopathologically and radiologically proven curative resection, obviating the need for further intervention. This is significant considering the local recurrence rates of 4.8-7% for expanded criteria lesions in Western populations, even on short-term follow up.

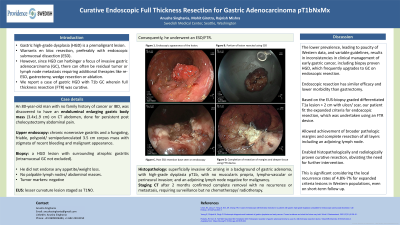
Figure: A. Endoscopic appearance of the lesion.
B. Portion of lesion resected using ESD.
C. Post-ESD resection base seen on endoscopy.
D. Completion of resection of margins and deeper tissue using FTR device.
B. Portion of lesion resected using ESD.
C. Post-ESD resection base seen on endoscopy.
D. Completion of resection of margins and deeper tissue using FTR device.
Disclosures:
Anusha Singhania indicated no relevant financial relationships.
Mohit Girotra indicated no relevant financial relationships.
Rajnish Mishra indicated no relevant financial relationships.
Anusha Singhania, MBBS1, Mohit Girotra, MD2, Rajnish Mishra, MD1. P1381 - Curative Endoscopic Full Thickness Resection for Gastric Adenocarcinoma pT1bNxMx, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
