Sunday Poster Session
Category: Esophagus
P0497 - Acute Esophageal Necrosis After Sequential Trimethoprim/Sulfamethoxazole Administration
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Karla M. Hernandez Mendiola, MD
Berkshire Medical Center
Pittsfield, MA
Presenting Author(s)
Karla M. Hernandez Mendiola, MD, Amna Rehman, MD, Anahit Muradyan, MD
Berkshire Medical Center, Pittsfield, MA
Introduction: Acute esophageal necrosis (AEN) is rare and potentially catastrophic. Although AEN pathophysiology is poorly understood, the etiology appears multifactorial. Risk factors include cardiovascular disease, HTN, atherosclerosis, diabetes, alcohol abuse, liver disease, renal failure, and GERD. Dysphagia, odynophagia, hematemesis, and abdominal pain are typical symptoms. AEN has rarely been reported to occur after antibiotic treatment, and only one report has described AEN after trimethoprim/ sulfamethoxazole (TMP/SMX) therapy.
Case Description/Methods: We describe here a case of AEN in a 75-year-old African American man with a history of essential hypertension, type 2 diabetes, GERD, and congestive heart failure. The patient presented hemodynamically and metabolically stable, showing mental status changes secondary to a urinary tract infection. TMP/SMX was started, but after two days, the patient developed nausea, vomiting, and dysphagia. No abdominal pain or hematemesis. Additionally, nephrotoxicity (creatinine 1.5) was noted, prompting TMP/SMX discontinuation. On exam, the abdomen was soft and non-tender, with no guarding or rebound, but abdominal distention was significant. During the next five days, dysphagia and vomiting worsened. Pantoprazole 40 mg IV BID and liquid diet were instituted.
Abdominal X-ray and CT scan, respectively, suggested significant gastroparesis, duodenitis, and a reactive jejunal ileus. Leukocytosis of 22.3 k/mm3 was noted.
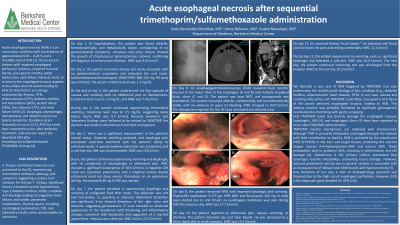
An esophagogastroduodenoscopy (EGD) showed black necrotic mucosa in the distal third of the esophagus (images A and B) and several duodenal ulcers (images C and D). The patient remained NPO, and pantoprazole administration was maintained. Over the next seven days, the patient showed a gradual improvement in dysphagia and vomiting, tolerating the transition to a liquid and soft diet allowing his discharge.
Discussion: The case report presented here is the second report in the literature describing AEN triggered by TMP/SMX treatment. In this case, TMP/SMX-induced nausea and vomiting could cause acid damage to a weakened and poorly perfused esophageal mucosa, triggering a chain of events leading to AEN. Idiosyncratic SMX toxicity could also cause AEN. SMX is activated by the cytochrome P450 (CYP2C9) in the liver and target tissues. Reactive oxygen species bind to proteins/DNA resulting in inflammation and cell damage. Conditions reducing glutathione anti-scavenger activity appear to increase the risk for idiosyncratic SMX toxicity.

Disclosures:
Karla M. Hernandez Mendiola, MD, Amna Rehman, MD, Anahit Muradyan, MD. P0497 - Acute Esophageal Necrosis After Sequential Trimethoprim/Sulfamethoxazole Administration, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Berkshire Medical Center, Pittsfield, MA
Introduction: Acute esophageal necrosis (AEN) is rare and potentially catastrophic. Although AEN pathophysiology is poorly understood, the etiology appears multifactorial. Risk factors include cardiovascular disease, HTN, atherosclerosis, diabetes, alcohol abuse, liver disease, renal failure, and GERD. Dysphagia, odynophagia, hematemesis, and abdominal pain are typical symptoms. AEN has rarely been reported to occur after antibiotic treatment, and only one report has described AEN after trimethoprim/ sulfamethoxazole (TMP/SMX) therapy.
Case Description/Methods: We describe here a case of AEN in a 75-year-old African American man with a history of essential hypertension, type 2 diabetes, GERD, and congestive heart failure. The patient presented hemodynamically and metabolically stable, showing mental status changes secondary to a urinary tract infection. TMP/SMX was started, but after two days, the patient developed nausea, vomiting, and dysphagia. No abdominal pain or hematemesis. Additionally, nephrotoxicity (creatinine 1.5) was noted, prompting TMP/SMX discontinuation. On exam, the abdomen was soft and non-tender, with no guarding or rebound, but abdominal distention was significant. During the next five days, dysphagia and vomiting worsened. Pantoprazole 40 mg IV BID and liquid diet were instituted.
Abdominal X-ray and CT scan, respectively, suggested significant gastroparesis, duodenitis, and a reactive jejunal ileus. Leukocytosis of 22.3 k/mm3 was noted.
An esophagogastroduodenoscopy (EGD) showed black necrotic mucosa in the distal third of the esophagus (images A and B) and several duodenal ulcers (images C and D). The patient remained NPO, and pantoprazole administration was maintained. Over the next seven days, the patient showed a gradual improvement in dysphagia and vomiting, tolerating the transition to a liquid and soft diet allowing his discharge.
Discussion: The case report presented here is the second report in the literature describing AEN triggered by TMP/SMX treatment. In this case, TMP/SMX-induced nausea and vomiting could cause acid damage to a weakened and poorly perfused esophageal mucosa, triggering a chain of events leading to AEN. Idiosyncratic SMX toxicity could also cause AEN. SMX is activated by the cytochrome P450 (CYP2C9) in the liver and target tissues. Reactive oxygen species bind to proteins/DNA resulting in inflammation and cell damage. Conditions reducing glutathione anti-scavenger activity appear to increase the risk for idiosyncratic SMX toxicity.

Figure: Images A and B show esophageal mucosa necrosis with spontaneous bleeding.
Images C and D show multiple ulcers in the descending duodenum.
Images C and D show multiple ulcers in the descending duodenum.
Disclosures:
Karla Hernandez Mendiola indicated no relevant financial relationships.
Amna Rehman indicated no relevant financial relationships.
Anahit Muradyan indicated no relevant financial relationships.
Karla M. Hernandez Mendiola, MD, Amna Rehman, MD, Anahit Muradyan, MD. P0497 - Acute Esophageal Necrosis After Sequential Trimethoprim/Sulfamethoxazole Administration, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
