Sunday Poster Session
Category: Biliary/Pancreas
P0066 - ACEi-ing It! Discovering a Rare Case of Lisinopril-Induced Pancreatitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Anusha Majagi, MD
Detroit Medical Center/Wayne State University
Detroit, MI
Presenting Author(s)
Anusha Majagi, MD1, Aabid Mohiuddin, DO1, Majd Khadra, MD1, TJ L. Wilson, MD1, Tooba Tariq, MD1, Bashar Mohamad, MD2
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State University, Detroit, MI
Introduction: Acute pancreatitis (AP) is one of the most common gastrointestinal diagnoses for inpatient admissions. While alcohol and gallstones are the most common etiologies of AP, medications can also cause inflammation of the pancreas. Lisinopril, an angiotensin-converting enzyme inhibitor (ACEi) has been documented in literature as being a rare cause of AP. An extensive literature review revealed only two other reports documenting necrotizing pancreatitis secondary to lisinopril use.
Case Description/Methods: A 55-year-old male was admitted for epigastric pain, nausea, and poor oral intake. He had similar, recurring episodes for a year from pancreatitis flares. Medical history included hypertension, type 2 diabetes mellitus, and peripheral artery disease. Surgical history included cholecystectomy. Home medications included lisinopril 10 mg daily, glipizide 2.5 mg daily, metformin 500 mg BID, cilostazol 100 mg daily, simvastatin 10 mg daily, pantoprazole 40 mg twice daily, acetaminophen 500 mg q4h; patient was discontinued on glipizide after early AP episodes. He reported smoking two cigars and marijuana daily but denied history of alcohol use/abuse. Family history was negative for pancreatitis. Physical exam findings included epigastric pain to palpation with voluntary guarding. Findings of epigastric pain, leukocytosis of 16K, and lipase levels in the 4000s on admission made AP the likely diagnosis. Negative or normal laboratory studies include electrolytes, liver function tests, IgG4, lipid profile, urinalysis, ECG, and chest X-Ray. MRI-cholangiopancreatography confirmed AP with necrosis (less than 30%) in the body of the pancreas. Normal biliary duct with absence of gallstones was noted. Thorough electronic health record review and patient interview revealed the patient was prescribed lisinopril a year ago when his AP symptoms began. Upon discontinuing lisinopril, his abdominal pain was greatly improved in subsequent outpatient follow-ups.
Discussion: Drug-induced AP is less than 5% of all AP cases, with lisinopril being a rare inciting agent. No clear link is established between ACEi and AP, but proposed mechanisms include pancreatic autodigestion due to bradykinin-induced ductal obstruction and inhibition of angiotensin II receptors causing dysregulation of pancreatic enzymes. When working up etiologies of AP, medication reconciliation should be performed to assess for offending agents. This case shows that while rare, ACEi should be considered in the differential in patients presenting with AP.

Disclosures:
Anusha Majagi, MD1, Aabid Mohiuddin, DO1, Majd Khadra, MD1, TJ L. Wilson, MD1, Tooba Tariq, MD1, Bashar Mohamad, MD2. P0066 - ACEi-ing It! Discovering a Rare Case of Lisinopril-Induced Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State University, Detroit, MI
Introduction: Acute pancreatitis (AP) is one of the most common gastrointestinal diagnoses for inpatient admissions. While alcohol and gallstones are the most common etiologies of AP, medications can also cause inflammation of the pancreas. Lisinopril, an angiotensin-converting enzyme inhibitor (ACEi) has been documented in literature as being a rare cause of AP. An extensive literature review revealed only two other reports documenting necrotizing pancreatitis secondary to lisinopril use.
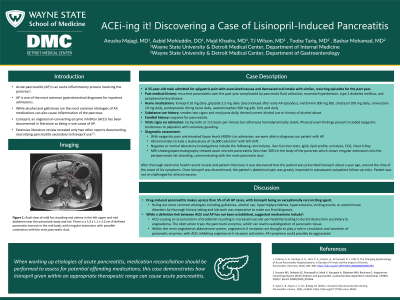
Case Description/Methods: A 55-year-old male was admitted for epigastric pain, nausea, and poor oral intake. He had similar, recurring episodes for a year from pancreatitis flares. Medical history included hypertension, type 2 diabetes mellitus, and peripheral artery disease. Surgical history included cholecystectomy. Home medications included lisinopril 10 mg daily, glipizide 2.5 mg daily, metformin 500 mg BID, cilostazol 100 mg daily, simvastatin 10 mg daily, pantoprazole 40 mg twice daily, acetaminophen 500 mg q4h; patient was discontinued on glipizide after early AP episodes. He reported smoking two cigars and marijuana daily but denied history of alcohol use/abuse. Family history was negative for pancreatitis. Physical exam findings included epigastric pain to palpation with voluntary guarding. Findings of epigastric pain, leukocytosis of 16K, and lipase levels in the 4000s on admission made AP the likely diagnosis. Negative or normal laboratory studies include electrolytes, liver function tests, IgG4, lipid profile, urinalysis, ECG, and chest X-Ray. MRI-cholangiopancreatography confirmed AP with necrosis (less than 30%) in the body of the pancreas. Normal biliary duct with absence of gallstones was noted. Thorough electronic health record review and patient interview revealed the patient was prescribed lisinopril a year ago when his AP symptoms began. Upon discontinuing lisinopril, his abdominal pain was greatly improved in subsequent outpatient follow-ups.
Discussion: Drug-induced AP is less than 5% of all AP cases, with lisinopril being a rare inciting agent. No clear link is established between ACEi and AP, but proposed mechanisms include pancreatic autodigestion due to bradykinin-induced ductal obstruction and inhibition of angiotensin II receptors causing dysregulation of pancreatic enzymes. When working up etiologies of AP, medication reconciliation should be performed to assess for offending agents. This case shows that while rare, ACEi should be considered in the differential in patients presenting with AP.

Figure: MRI-cholangiopancreatography image showing acute necrotic pancreatitis (less than 30%) in the body of the pancreas which has irregular extensions into the peripancreatic fat stranding and appears to be in communication with the main pancreatic duct. The large cystic lesion measuring 8 x 6.6 x 6 cm represents walled-off necrosis.
Disclosures:
Anusha Majagi indicated no relevant financial relationships.
Aabid Mohiuddin indicated no relevant financial relationships.
Majd Khadra indicated no relevant financial relationships.
TJ Wilson indicated no relevant financial relationships.
Tooba Tariq indicated no relevant financial relationships.
Bashar Mohamad indicated no relevant financial relationships.
Anusha Majagi, MD1, Aabid Mohiuddin, DO1, Majd Khadra, MD1, TJ L. Wilson, MD1, Tooba Tariq, MD1, Bashar Mohamad, MD2. P0066 - ACEi-ing It! Discovering a Rare Case of Lisinopril-Induced Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
