Monday Poster Session
Category: Esophagus
P1820 - Esophageal Aperistalsis: A Management Conundrum
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- HS
Hasan Saleh, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Hasan Saleh, MD1, Paul Travers, MD1, Kenneth DeVault, MD2, Brian Lacy, MD, PhD, FACG1, Maoyin Pang, MD, PhD2
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Florida, Jacksonville, FL
Introduction: Esophageal non-achalasia aperistalsis has limited studies and is difficult to manage leading to refractory gastroesophageal reflux and dysphagia. Etiology is often secondary to rare connective tissue diseases like scleroderma. Diagnosis is made through manometry. Fundoplication is a surgical option for severe, intractable reflux.
Methods: In this retrospective case series, patients with non-achalasia aperistalsis were evaluated based on esophageal manometry per Chicago Classification. Demographics, upper GI symptoms, underlying diagnosis, objective studies including esophageal manometry, endoscopy, and esophageal pH testing, as well as medical management (PPI, H2 blockers, etc.) and surgical interventions including fundoplication type were recorded. Outcomes were measured as symptom resolution, new symptoms or complications.
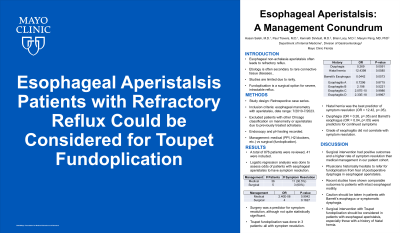
Results: A total of 876 patients were reviewed, 41 were included. A total of 36 patients underwent medical management, 11 had symptom resolution (30.5%). The remaining 5 patients underwent fundoplication, 3 of which had symptom resolution (60%). Toupet fundoplication technique was done in 3 patients, all with symptom resolution. The other two surgical techniques were peroral endoscopic myotomy with fundoplication and transoral incisionless fundoplication resulting in persistent symptoms. History of hiatal hernia was the best predictor for symptom resolution (OR = 12.42, p=.05). Dysphagia was the only predominant symptom that was a predictor for continued symptoms, calculated as decreased odds of resolution (OR = 0.26, p=.05). Barrett’s esophagus seen on endoscopy was a predictor for continued symptoms, calculated again as decreased odds of resolution (OR = 0.04, p=.05). Management strategy involving surgery was a predictor for symptom resolution, although not statistically significant (OR = 4, p=0.16). No surgical complications were seen.
Discussion: Surgical intervention had positive outcomes and a higher rate of symptom resolution than medical management in our patient cohort. Larger studies are difficult due to rarity of disease. Physicians historically hesitate to operate from perceived postoperative dysphagia, but recent studies have shown comparable outcomes to patients with intact esophageal motility. Caution should be taken in patients with Barrett’s esophagus or symptomatic dysphagia. Surgical intervention with Toupet fundoplication should be considered in patients with esophageal aperistalsis, especially those with a history of hiatal hernia.
Disclosures:
Hasan Saleh, MD1, Paul Travers, MD1, Kenneth DeVault, MD2, Brian Lacy, MD, PhD, FACG1, Maoyin Pang, MD, PhD2. P1820 - Esophageal Aperistalsis: A Management Conundrum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Florida, Jacksonville, FL
Introduction: Esophageal non-achalasia aperistalsis has limited studies and is difficult to manage leading to refractory gastroesophageal reflux and dysphagia. Etiology is often secondary to rare connective tissue diseases like scleroderma. Diagnosis is made through manometry. Fundoplication is a surgical option for severe, intractable reflux.
Methods: In this retrospective case series, patients with non-achalasia aperistalsis were evaluated based on esophageal manometry per Chicago Classification. Demographics, upper GI symptoms, underlying diagnosis, objective studies including esophageal manometry, endoscopy, and esophageal pH testing, as well as medical management (PPI, H2 blockers, etc.) and surgical interventions including fundoplication type were recorded. Outcomes were measured as symptom resolution, new symptoms or complications.
Results: A total of 876 patients were reviewed, 41 were included. A total of 36 patients underwent medical management, 11 had symptom resolution (30.5%). The remaining 5 patients underwent fundoplication, 3 of which had symptom resolution (60%). Toupet fundoplication technique was done in 3 patients, all with symptom resolution. The other two surgical techniques were peroral endoscopic myotomy with fundoplication and transoral incisionless fundoplication resulting in persistent symptoms. History of hiatal hernia was the best predictor for symptom resolution (OR = 12.42, p=.05). Dysphagia was the only predominant symptom that was a predictor for continued symptoms, calculated as decreased odds of resolution (OR = 0.26, p=.05). Barrett’s esophagus seen on endoscopy was a predictor for continued symptoms, calculated again as decreased odds of resolution (OR = 0.04, p=.05). Management strategy involving surgery was a predictor for symptom resolution, although not statistically significant (OR = 4, p=0.16). No surgical complications were seen.
Discussion: Surgical intervention had positive outcomes and a higher rate of symptom resolution than medical management in our patient cohort. Larger studies are difficult due to rarity of disease. Physicians historically hesitate to operate from perceived postoperative dysphagia, but recent studies have shown comparable outcomes to patients with intact esophageal motility. Caution should be taken in patients with Barrett’s esophagus or symptomatic dysphagia. Surgical intervention with Toupet fundoplication should be considered in patients with esophageal aperistalsis, especially those with a history of hiatal hernia.
Disclosures:
Hasan Saleh indicated no relevant financial relationships.
Paul Travers indicated no relevant financial relationships.
Kenneth DeVault indicated no relevant financial relationships.
Brian Lacy: AbbVie, Inc. – Advisory Committee/Board Member, Investigator-initiated funding. Ardelyx, Inc. – Advisory Committee/Board Member. Bausch – Investigator-initiated funding. Gernelli – Advisory Committee/Board Member. Ironwood Pharmaceuticals Inc. – Advisory Committee/Board Member, Investigator-initiated funding. Salix – Advisory Committee/Board Member, Investigator-initiated funding. Sanofi – Advisory Committee/Board Member.
Maoyin Pang indicated no relevant financial relationships.
Hasan Saleh, MD1, Paul Travers, MD1, Kenneth DeVault, MD2, Brian Lacy, MD, PhD, FACG1, Maoyin Pang, MD, PhD2. P1820 - Esophageal Aperistalsis: A Management Conundrum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
