Monday Poster Session
Category: Esophagus
P1828 - Short Segment Barrett’s May Have More Rapid Surface Progression Than Long Segment Barrett’s Over Time
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Christopher J. Costa, MD
University of Connecticut Health Center
Farmington, CT
Presenting Author(s)
Christopher J. Costa, MD1, Houman Rezaizadeh, MD2, John Birk, MD, FACG1
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut, Farmington, CT
Introduction: Barrett’s esophagus (BE) is a frequently encountered clinical entity in individuals with GERD. The incidence and prevalence have been increasing in the US, underscoring the importance of detection and surveillance. Some data suggests that acid suppression of intestinal metaplasia improves mortality, but it is unclear if it improves pathological progression. Less is known about predictive factors in the surface progression of non-dysplastic BE. We report on a retrospective analysis of factors influencing surface progression of non-dysplastic BE based on patient endoscopy reports conducted at an academic center over a 5-year period.
Methods: Patient demographics including Age, Sex, BMI, PPI treatment and BE segment length at initial endoscopy, were collected. Both circumferential (C) and longitudinal extent (M) extent of BE lesion as defined by Prague criteria were evaluated. Since follow-up time was variable, changes in C and M were standardized by taking the difference between final and initial measurement and dividing by follow-up time in years to come up with a yearly change variable for each case. Short segment was defined as M < 3cm.
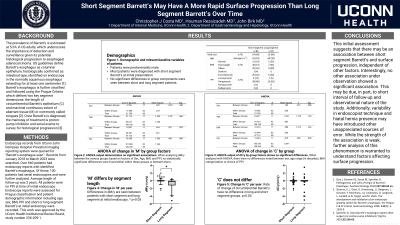
Results: 100 patients with repeat endoscopies were identified with average follow-up time of 2.1 years. Patients were 68% male, had an average age of 61±10 at initial endoscopy, BMI average was 29.7±5.7, with 80% of patients having short segment BE at initial endoscopy. Variables were compared using ANOVA analysis via SPSS. The two groups, Short BE and Long BE were compared using the Mann-Whitney U test. No significant associations were seen between surface progression of C per year(dC/y) or M per year (dM/y) with age, sex, BMI, or segment length at initial endoscopy. However, there was a significant association seen between dM/y and BE segment length at initial endoscopy. Mean ranks for short (53.84) and long (37.15) were compared, these were significantly different (U=533.00, p=0.011) with an Effect Size (r) of 0.2551. This suggests that the initial segment length is a slight but significant factor in surface progression of BE lesions with short segment BE having a more rapid progression than long segment over time.
Discussion: This initial work provides a first step in associating clinical risk factors for surface progression of BE lesions. Further work on the combinatorial effects of various demographic and treatment factors is needed but this study suggests that short segment BE has some noteworthy features.

Disclosures:
Christopher J. Costa, MD1, Houman Rezaizadeh, MD2, John Birk, MD, FACG1. P1828 - Short Segment Barrett’s May Have More Rapid Surface Progression Than Long Segment Barrett’s Over Time, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut, Farmington, CT
Introduction: Barrett’s esophagus (BE) is a frequently encountered clinical entity in individuals with GERD. The incidence and prevalence have been increasing in the US, underscoring the importance of detection and surveillance. Some data suggests that acid suppression of intestinal metaplasia improves mortality, but it is unclear if it improves pathological progression. Less is known about predictive factors in the surface progression of non-dysplastic BE. We report on a retrospective analysis of factors influencing surface progression of non-dysplastic BE based on patient endoscopy reports conducted at an academic center over a 5-year period.
Methods: Patient demographics including Age, Sex, BMI, PPI treatment and BE segment length at initial endoscopy, were collected. Both circumferential (C) and longitudinal extent (M) extent of BE lesion as defined by Prague criteria were evaluated. Since follow-up time was variable, changes in C and M were standardized by taking the difference between final and initial measurement and dividing by follow-up time in years to come up with a yearly change variable for each case. Short segment was defined as M < 3cm.
Results: 100 patients with repeat endoscopies were identified with average follow-up time of 2.1 years. Patients were 68% male, had an average age of 61±10 at initial endoscopy, BMI average was 29.7±5.7, with 80% of patients having short segment BE at initial endoscopy. Variables were compared using ANOVA analysis via SPSS. The two groups, Short BE and Long BE were compared using the Mann-Whitney U test. No significant associations were seen between surface progression of C per year(dC/y) or M per year (dM/y) with age, sex, BMI, or segment length at initial endoscopy. However, there was a significant association seen between dM/y and BE segment length at initial endoscopy. Mean ranks for short (53.84) and long (37.15) were compared, these were significantly different (U=533.00, p=0.011) with an Effect Size (r) of 0.2551. This suggests that the initial segment length is a slight but significant factor in surface progression of BE lesions with short segment BE having a more rapid progression than long segment over time.
Discussion: This initial work provides a first step in associating clinical risk factors for surface progression of BE lesions. Further work on the combinatorial effects of various demographic and treatment factors is needed but this study suggests that short segment BE has some noteworthy features.

Figure: Figure 1: Medians of Short and Long segment groups' change in M over time. Whiskers are 10-90th percentiles. *p<0.05
Disclosures:
Christopher Costa indicated no relevant financial relationships.
Houman Rezaizadeh: AstraZeneca – Stock-publicly held company(excluding mutual/index funds). Regeneron – Advisory Committee/Board Member, Speakers Bureau. Sanofi – Advisory Committee/Board Member. Skope Inc – Consultant, Stock Options, Stock-privately held company.
John Birk indicated no relevant financial relationships.
Christopher J. Costa, MD1, Houman Rezaizadeh, MD2, John Birk, MD, FACG1. P1828 - Short Segment Barrett’s May Have More Rapid Surface Progression Than Long Segment Barrett’s Over Time, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
