Monday Poster Session
Category: Esophagus
P1859 - Pemphigus Vulgaris and Esophageal Dissecans: A Rare Association Explored
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Kazi N. Khan, MD
Aurora Healthcare
Milwaukee, WI
Presenting Author(s)
Kazi Khan, MD1, Mohammad Aasim Khan, MBBS2, Abdulaziz Siddiqui, MD1, Matthew Kobeszko, MD, MBA, MSc1, Aboud Affi, MD1, Biana Leybishkis, MD1
1Aurora Healthcare, Milwaukee, WI; 2Khyber Medical College & Advocate Health Aurora St. Luke’s Medical Center, Milwaukee, WI
Introduction: Esophageal Dissecans Superficialis (EDS) is a rare condition characterized by the separation of the esophageal mucosa and submucosa, leading to erosive esophagitis. This case report highlights the uncommon association between EDS and Pemphigus Vulgaris (PV), a bullous autoimmune disease. We present the clinical features, diagnostic challenges, and treatment approach in a patient with concurrent PV and EDS, shedding light on this intriguing connection.
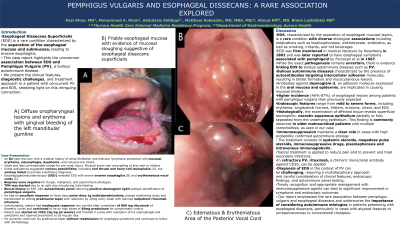
Case Description/Methods: An 82-year-old man with a medical history of atrial fibrillation and follicular lymphoma presented with mucosal erythema, dysphagia, dysphonia, and reduced oral intake. Initial evaluations suggested various possibilities, including oral thrush and hairy-cell leukoplakia (A), but workup failed to provide a definitive diagnosis. Esophagogastroduodenoscopy (EGD) revealed EDS with severe erosive esophagitis (B) and erythematous vocal cords (C). Biopsies were negative for fungal, malignant, and autoimmune etiologies. Further investigation led to the identification of pemphigus vulgaris via autoantibody panel testing. The patient had an excellent response to pulse-dose 1mg/kg methylprednisolone and transitioned to oral prednisone taper with outpatient rituximab infusions. Due to non-adherence, he currently continues his prednisone taper 3 months later without readmission for dysphagia symptoms and follows with dermatology.
Discussion: EDS, characterized by the separation of esophageal mucosal layers, is a rare condition with diverse etiological associations. While the exact pathogenesis remains uncertain, there is evidence linking EDS to bullous autoimmune diseases such as PV. The presence of esophageal symptoms in patients with PV ranges from 46-87%. Diagnosis of EDS in the context of PV can be challenging, requiring a multidisciplinary approach and careful consideration of clinical features, endoscopic findings, and autoimmune panel testing. Timely recognition and appropriate management with immunosuppressive agents can lead to significant improvement in symptoms and endoscopic outcomes.
Our report emphasizes the rare association between pemphigus vulgaris and esophageal dissecans. It underscores the importance of considering autoimmune etiologies in patients presenting with esophageal dissecans, particularly in cases with atypical features or unresponsiveness to conventional therapies. Reporting this rare association will facilitate improved diagnostic accuracy and tailored treatment strategies in the future.

Disclosures:
Kazi Khan, MD1, Mohammad Aasim Khan, MBBS2, Abdulaziz Siddiqui, MD1, Matthew Kobeszko, MD, MBA, MSc1, Aboud Affi, MD1, Biana Leybishkis, MD1. P1859 - Pemphigus Vulgaris and Esophageal Dissecans: A Rare Association Explored, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Aurora Healthcare, Milwaukee, WI; 2Khyber Medical College & Advocate Health Aurora St. Luke’s Medical Center, Milwaukee, WI
Introduction: Esophageal Dissecans Superficialis (EDS) is a rare condition characterized by the separation of the esophageal mucosa and submucosa, leading to erosive esophagitis. This case report highlights the uncommon association between EDS and Pemphigus Vulgaris (PV), a bullous autoimmune disease. We present the clinical features, diagnostic challenges, and treatment approach in a patient with concurrent PV and EDS, shedding light on this intriguing connection.
Case Description/Methods: An 82-year-old man with a medical history of atrial fibrillation and follicular lymphoma presented with mucosal erythema, dysphagia, dysphonia, and reduced oral intake. Initial evaluations suggested various possibilities, including oral thrush and hairy-cell leukoplakia (A), but workup failed to provide a definitive diagnosis. Esophagogastroduodenoscopy (EGD) revealed EDS with severe erosive esophagitis (B) and erythematous vocal cords (C). Biopsies were negative for fungal, malignant, and autoimmune etiologies. Further investigation led to the identification of pemphigus vulgaris via autoantibody panel testing. The patient had an excellent response to pulse-dose 1mg/kg methylprednisolone and transitioned to oral prednisone taper with outpatient rituximab infusions. Due to non-adherence, he currently continues his prednisone taper 3 months later without readmission for dysphagia symptoms and follows with dermatology.
Discussion: EDS, characterized by the separation of esophageal mucosal layers, is a rare condition with diverse etiological associations. While the exact pathogenesis remains uncertain, there is evidence linking EDS to bullous autoimmune diseases such as PV. The presence of esophageal symptoms in patients with PV ranges from 46-87%. Diagnosis of EDS in the context of PV can be challenging, requiring a multidisciplinary approach and careful consideration of clinical features, endoscopic findings, and autoimmune panel testing. Timely recognition and appropriate management with immunosuppressive agents can lead to significant improvement in symptoms and endoscopic outcomes.
Our report emphasizes the rare association between pemphigus vulgaris and esophageal dissecans. It underscores the importance of considering autoimmune etiologies in patients presenting with esophageal dissecans, particularly in cases with atypical features or unresponsiveness to conventional therapies. Reporting this rare association will facilitate improved diagnostic accuracy and tailored treatment strategies in the future.

Figure: A) Diffuse oropharyngeal lesions and erythema with gingival bleeding of the left mandibular gumline
B) Friable esophageal mucosa with evidence of mucosal sloughing suggestive of esophageal dissecans superficialis
C) Edematous/Erythematous Area Adjacent to Posterior Vocal Cord
B) Friable esophageal mucosa with evidence of mucosal sloughing suggestive of esophageal dissecans superficialis
C) Edematous/Erythematous Area Adjacent to Posterior Vocal Cord
Disclosures:
Kazi Khan indicated no relevant financial relationships.
Mohammad Aasim Khan indicated no relevant financial relationships.
Abdulaziz Siddiqui indicated no relevant financial relationships.
Matthew Kobeszko indicated no relevant financial relationships.
Aboud Affi indicated no relevant financial relationships.
Biana Leybishkis indicated no relevant financial relationships.
Kazi Khan, MD1, Mohammad Aasim Khan, MBBS2, Abdulaziz Siddiqui, MD1, Matthew Kobeszko, MD, MBA, MSc1, Aboud Affi, MD1, Biana Leybishkis, MD1. P1859 - Pemphigus Vulgaris and Esophageal Dissecans: A Rare Association Explored, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
