Monday Poster Session
Category: Esophagus
P1865 - Dysphagia Megalatriensis: An Atypical Case of Heart Failure Exacerbation
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Abhishek A. Alur, MD, MBA
Loyola University Medical Center
Maywood, IL
Presenting Author(s)
Abhishek A. Alur, MD, MBA1, Judie Hoilat, MD2, Gilles Hoilat, MD3, Bianca Varda, MD1, Judy Trieu, MD4, Mukund Venu, MD1
1Loyola University Medical Center, Maywood, IL; 2Medical College of Wisconsin, Milwaukee, WI; 3University of Iowa College of Medicine, Iowa City, IA; 4University of North Carolina School of Medicine, Chapel Hill, NC
Introduction: Dysphagia megalatriensis (cardiac dysphagia) is difficulty swallowing due to external compression of the esophagus by an enlarged left atrium. Most cases of cardiac dysphagia published in literature occur in the setting of mitral stenosis and require surgical management. We present a unique case of cardiac dysphagia due to heart failure (HF) exacerbation that resolved with medical management.
Case Description/Methods: A 96 year old male with a history of hypertension, coronary artery disease, HF with preserved ejection fraction, and chronic kidney disease presented with sudden onset of difficulty swallowing with dysphagia to both solids and liquids. He denied shortness of breath. He had a new oxygen requirement with otherwise normal vitals. Physical exam was remarkable for bilateral lung base crackles and BLE edema.
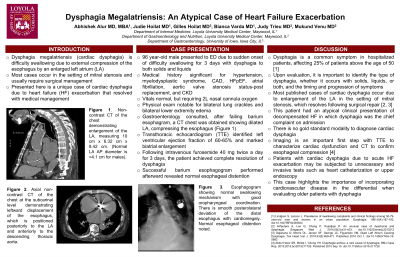
Gastroenterology was consulted and initially attempted a barium esophogram, but the patient did not tolerate due to vomiting. Thus, a computed tomography (CT) of the chest and abdomen was obtained, revealing a dilated LA compressing the esophagus. An transthoracic echocardiogram (TTE) demonstrated a normal ejection fraction, biatrial enlargement, and mitral valve regurgitation, suggesting an acute HF exacerbation. Remarkably, his dysphagia resolved completely after receiving three days of intravenous diuresis.
Discussion: Dysphagia is a common symptom in hospitalized patients, affecting 25% of patients above the age of 50. Upon evaluation, it is important to identify the type of dysphagia, whether it occurs with solids, liquids, or both, and the timing and progression of symptoms. Disorders leading to dysphagia can be classified by organ system or by mechanism.
Most published cases of cardiac dysphagia occur due to enlargement of the LA in the setting of mitral stenosis, which resolves following surgical intervention. This case report illustrates an atypical presentation of cardiac dysphagia: an external compression of the esophagus by an enlarged LA due to an acute HF exacerbation.
There is no gold standard modality to diagnose cardiac dysphagia. Imaging is an important first step with TTE to characterize cardiac dysfunction and CT to confirm esophageal compression. Patients presenting with cardiac dysphagia due to acute HF exacerbation may be subjected to unnecessary and invasive tests such as heart catheterization or upper endoscopy. This study highlights the importance of incorporating cardiovascular disease in the differential when evaluating older patients with dysphagia.

Disclosures:
Abhishek A. Alur, MD, MBA1, Judie Hoilat, MD2, Gilles Hoilat, MD3, Bianca Varda, MD1, Judy Trieu, MD4, Mukund Venu, MD1. P1865 - Dysphagia Megalatriensis: An Atypical Case of Heart Failure Exacerbation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Loyola University Medical Center, Maywood, IL; 2Medical College of Wisconsin, Milwaukee, WI; 3University of Iowa College of Medicine, Iowa City, IA; 4University of North Carolina School of Medicine, Chapel Hill, NC
Introduction: Dysphagia megalatriensis (cardiac dysphagia) is difficulty swallowing due to external compression of the esophagus by an enlarged left atrium. Most cases of cardiac dysphagia published in literature occur in the setting of mitral stenosis and require surgical management. We present a unique case of cardiac dysphagia due to heart failure (HF) exacerbation that resolved with medical management.
Case Description/Methods: A 96 year old male with a history of hypertension, coronary artery disease, HF with preserved ejection fraction, and chronic kidney disease presented with sudden onset of difficulty swallowing with dysphagia to both solids and liquids. He denied shortness of breath. He had a new oxygen requirement with otherwise normal vitals. Physical exam was remarkable for bilateral lung base crackles and BLE edema.
Gastroenterology was consulted and initially attempted a barium esophogram, but the patient did not tolerate due to vomiting. Thus, a computed tomography (CT) of the chest and abdomen was obtained, revealing a dilated LA compressing the esophagus. An transthoracic echocardiogram (TTE) demonstrated a normal ejection fraction, biatrial enlargement, and mitral valve regurgitation, suggesting an acute HF exacerbation. Remarkably, his dysphagia resolved completely after receiving three days of intravenous diuresis.
Discussion: Dysphagia is a common symptom in hospitalized patients, affecting 25% of patients above the age of 50. Upon evaluation, it is important to identify the type of dysphagia, whether it occurs with solids, liquids, or both, and the timing and progression of symptoms. Disorders leading to dysphagia can be classified by organ system or by mechanism.
Most published cases of cardiac dysphagia occur due to enlargement of the LA in the setting of mitral stenosis, which resolves following surgical intervention. This case report illustrates an atypical presentation of cardiac dysphagia: an external compression of the esophagus by an enlarged LA due to an acute HF exacerbation.
There is no gold standard modality to diagnose cardiac dysphagia. Imaging is an important first step with TTE to characterize cardiac dysfunction and CT to confirm esophageal compression. Patients presenting with cardiac dysphagia due to acute HF exacerbation may be subjected to unnecessary and invasive tests such as heart catheterization or upper endoscopy. This study highlights the importance of incorporating cardiovascular disease in the differential when evaluating older patients with dysphagia.

Figure: Esophagogram showing normal swallowing mechanism with good oropharyngeal coordination. There is smooth posterolateral deviation of the distal esophagus with cardiomegaly. Normal esophageal distention is noted without stricture or extrinsic or
intrinsic mass.
intrinsic mass.
Disclosures:
Abhishek Alur indicated no relevant financial relationships.
Judie Hoilat indicated no relevant financial relationships.
Gilles Hoilat indicated no relevant financial relationships.
Bianca Varda indicated no relevant financial relationships.
Judy Trieu indicated no relevant financial relationships.
Mukund Venu indicated no relevant financial relationships.
Abhishek A. Alur, MD, MBA1, Judie Hoilat, MD2, Gilles Hoilat, MD3, Bianca Varda, MD1, Judy Trieu, MD4, Mukund Venu, MD1. P1865 - Dysphagia Megalatriensis: An Atypical Case of Heart Failure Exacerbation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
