Monday Poster Session
Category: Esophagus
P1916 - A Tremendously Tortuous Time
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- CC
Charles P. Cavalaris, MD
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Charles P. Cavalaris, MD, Shreya Narayanan, MD, John Jacobs, MD
University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: Achalasia is classified as a disorder of esophagogastric junction (EGJ) outflow, requiring an elevated integrated relaxation pressure (IRP) in addition to aperistalsis on high-resolution esophageal manometry (HREM). While HREM is the most sensitive and specific test to secure the diagnosis of achalasia, there are cases where other diagnostic modalities may have important clinical utility. Herein, we present a case of end-stage achalasia that highlights the value of timed barium swallow (TBS) in disease management.
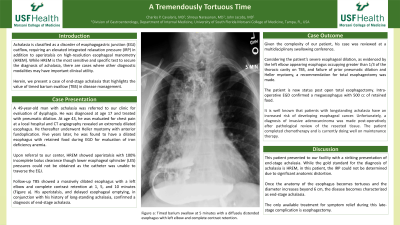
Case Description/Methods: A 49-year-old man with achalasia was referred to our clinic for evaluation of dysphagia. He was diagnosed at age 17 and treated with pneumatic dilation. At age 43, he was evaluated for chest pain at a local hospital and CT angiography revealed an extremely dilated esophagus. He thereafter underwent Heller myotomy with anterior fundoplication. Five years later, he was found to have a dilated esophagus with retained food during EGD for evaluation of iron deficiency anemia. Upon referral to our center, high-resolution esophageal manometry (HREM) showed aperistalsis with 100% incomplete bolus clearance though lower esophageal sphincter (LES) pressures could not be obtained as the catheter was unable to traverse the EGJ. Follow-up TBS showed a massively dilated esophagus with a left elbow and complete contrast retention at 1, 5, and 10 minutes (Figure a). His aperistalsis, and delayed esophageal emptying, in conjunction with his history of long-standing achalasia, confirmed a diagnosis of end-stage achalasia.
Discussion: This patient presented to our facility with a striking presentation of end-stage achalasia. While the gold standard for the diagnosis of achalasia is HREM, in this patient, the IRP could not be determined due to significant anatomic distortion. Once the anatomy of the esophagus becomes tortuous and the diameter increases beyond 6 cm, the disease becomes characterized as end-stage achalasia. The only available treatment for symptom relief during this late-stage complication is esophagectomy. Given the complexity of our patient, his case was reviewed at a multidisciplinary swallowing conference. Considering the patient’s severe esophageal dilation, as evidenced by the left elbow appearing esophagus occupying greater than 1/3 of the thoracic cavity on TBS, and failure of prior pneumatic dilations and Heller myotomy, a recommendation for total esophagectomy was made.

Disclosures:
Charles P. Cavalaris, MD, Shreya Narayanan, MD, John Jacobs, MD. P1916 - A Tremendously Tortuous Time, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: Achalasia is classified as a disorder of esophagogastric junction (EGJ) outflow, requiring an elevated integrated relaxation pressure (IRP) in addition to aperistalsis on high-resolution esophageal manometry (HREM). While HREM is the most sensitive and specific test to secure the diagnosis of achalasia, there are cases where other diagnostic modalities may have important clinical utility. Herein, we present a case of end-stage achalasia that highlights the value of timed barium swallow (TBS) in disease management.
Case Description/Methods: A 49-year-old man with achalasia was referred to our clinic for evaluation of dysphagia. He was diagnosed at age 17 and treated with pneumatic dilation. At age 43, he was evaluated for chest pain at a local hospital and CT angiography revealed an extremely dilated esophagus. He thereafter underwent Heller myotomy with anterior fundoplication. Five years later, he was found to have a dilated esophagus with retained food during EGD for evaluation of iron deficiency anemia. Upon referral to our center, high-resolution esophageal manometry (HREM) showed aperistalsis with 100% incomplete bolus clearance though lower esophageal sphincter (LES) pressures could not be obtained as the catheter was unable to traverse the EGJ. Follow-up TBS showed a massively dilated esophagus with a left elbow and complete contrast retention at 1, 5, and 10 minutes (Figure a). His aperistalsis, and delayed esophageal emptying, in conjunction with his history of long-standing achalasia, confirmed a diagnosis of end-stage achalasia.
Discussion: This patient presented to our facility with a striking presentation of end-stage achalasia. While the gold standard for the diagnosis of achalasia is HREM, in this patient, the IRP could not be determined due to significant anatomic distortion. Once the anatomy of the esophagus becomes tortuous and the diameter increases beyond 6 cm, the disease becomes characterized as end-stage achalasia. The only available treatment for symptom relief during this late-stage complication is esophagectomy. Given the complexity of our patient, his case was reviewed at a multidisciplinary swallowing conference. Considering the patient’s severe esophageal dilation, as evidenced by the left elbow appearing esophagus occupying greater than 1/3 of the thoracic cavity on TBS, and failure of prior pneumatic dilations and Heller myotomy, a recommendation for total esophagectomy was made.

Figure: Figure a: Timed barium swallow at 5 minutes with a diffusely distended esophagus with left elbow and complete contrast retention.
Disclosures:
Charles Cavalaris indicated no relevant financial relationships.
Shreya Narayanan indicated no relevant financial relationships.
John Jacobs indicated no relevant financial relationships.
Charles P. Cavalaris, MD, Shreya Narayanan, MD, John Jacobs, MD. P1916 - A Tremendously Tortuous Time, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
