Monday Poster Session
Category: Esophagus
P1918 - LAMS for Resistant Esophageal Anastomotic Strictures: A Novel Therapy
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Charmy Parikh, MD
North West Health
Chicago, IL
Presenting Author(s)
Charmy Parikh, MD, Raj Patel, MD, Anish Chopra, MD, Harpreet Singh, MD
North West Health, Chicago, IL
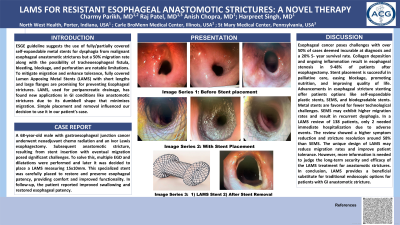
Introduction: ESGE guideline suggests the use of fully/partially covered self-expandable metal stents for dysphagia from malignant esophageal anastomotic strictures but a 50% migration rate along with the possibility of tracheoesophageal fistula, bleeding, blockage, and perforation are notable limitations. To mitigate migration and enhance tolerance, fully covered Lumen Apposing Metal Stents (LAMS) with short lengths and large flanges are promising for preventing Esophageal strictures. LAMS, used for peripancreatic drainage, has found new applications in GI conditions like anastomotic strictures due to its dumbbell shape that minimizes migration. Simple placement and removal influenced our decision to use it in our patient’s case.
Case Description/Methods: A 68-year-old male with gastroesophageal junction cancer underwent neoadjuvant chemoradiation and an Ivor Lewis esophagectomy. Subsequent anastomotic stricture, resulting from stent insertion with eventual migration posed significant challenges. To solve this, multiple EGD and dilatations were performed and later it was decided to place a LAMS measuring 15x10mm. This specialized stent was carefully placed to restore and preserve esophageal patency, providing comfort and improved functionality. In follow-up, the patient reported improved swallowing and restored esophageal patency.
Discussion: Esophageal cancer poses challenges with over 50% of cases deemed incurable at diagnosis and a 20% 5-year survival rate. Collagen deposition and ongoing inflammation result in esophageal stenosis in 9-48% of patients after esophagectomy. Stent placement is successful in palliative care, easing blockage, promoting nutrition, and improving quality of life. Advancements in esophageal stricture stenting offer patients options like self-expandable plastic stents, SEMS, and biodegradable stents. Metal stents are favored for fewer technological challenges. SEMS may exhibit higher migration rates and result in recurrent dysphagia. In a LAMS review of 138 patients, only 2 needed immediate hospitalization due to adverse events. The review showed a higher symptom reduction and stricture resolution around 58% than SEMS. The unique design of LAMS may reduce migration rates and improve patient tolerance. However, more information is needed to judge the long-term security and efficacy of the LAMS treatment for anastomotic strictures. In conclusion, LAMS provides a beneficial substitute for traditional endoscopic options for patients with GI anastomotic stricture.
Disclosures:
Charmy Parikh, MD, Raj Patel, MD, Anish Chopra, MD, Harpreet Singh, MD. P1918 - LAMS for Resistant Esophageal Anastomotic Strictures: A Novel Therapy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
North West Health, Chicago, IL
Introduction: ESGE guideline suggests the use of fully/partially covered self-expandable metal stents for dysphagia from malignant esophageal anastomotic strictures but a 50% migration rate along with the possibility of tracheoesophageal fistula, bleeding, blockage, and perforation are notable limitations. To mitigate migration and enhance tolerance, fully covered Lumen Apposing Metal Stents (LAMS) with short lengths and large flanges are promising for preventing Esophageal strictures. LAMS, used for peripancreatic drainage, has found new applications in GI conditions like anastomotic strictures due to its dumbbell shape that minimizes migration. Simple placement and removal influenced our decision to use it in our patient’s case.
Case Description/Methods: A 68-year-old male with gastroesophageal junction cancer underwent neoadjuvant chemoradiation and an Ivor Lewis esophagectomy. Subsequent anastomotic stricture, resulting from stent insertion with eventual migration posed significant challenges. To solve this, multiple EGD and dilatations were performed and later it was decided to place a LAMS measuring 15x10mm. This specialized stent was carefully placed to restore and preserve esophageal patency, providing comfort and improved functionality. In follow-up, the patient reported improved swallowing and restored esophageal patency.
Discussion: Esophageal cancer poses challenges with over 50% of cases deemed incurable at diagnosis and a 20% 5-year survival rate. Collagen deposition and ongoing inflammation result in esophageal stenosis in 9-48% of patients after esophagectomy. Stent placement is successful in palliative care, easing blockage, promoting nutrition, and improving quality of life. Advancements in esophageal stricture stenting offer patients options like self-expandable plastic stents, SEMS, and biodegradable stents. Metal stents are favored for fewer technological challenges. SEMS may exhibit higher migration rates and result in recurrent dysphagia. In a LAMS review of 138 patients, only 2 needed immediate hospitalization due to adverse events. The review showed a higher symptom reduction and stricture resolution around 58% than SEMS. The unique design of LAMS may reduce migration rates and improve patient tolerance. However, more information is needed to judge the long-term security and efficacy of the LAMS treatment for anastomotic strictures. In conclusion, LAMS provides a beneficial substitute for traditional endoscopic options for patients with GI anastomotic stricture.
Disclosures:
Charmy Parikh indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Anish Chopra indicated no relevant financial relationships.
Harpreet Singh indicated no relevant financial relationships.
Charmy Parikh, MD, Raj Patel, MD, Anish Chopra, MD, Harpreet Singh, MD. P1918 - LAMS for Resistant Esophageal Anastomotic Strictures: A Novel Therapy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
