Monday Poster Session
Category: Esophagus
P1924 - The Black Esophagus - A Case of Acute Esophageal Necrosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- GS
Gurdeep Singh, DO
AdventHealth
Orlando, FL
Presenting Author(s)
Gurdeep Singh, DO, Arooj Mian, MD, Abdul Mohammed, MD, Swotantra Gautam, MD, Neethi Paranji, MD
AdventHealth, Orlando, FL
Introduction: Acute esophageal necrosis (AEN), also known as “the black esophagus,” refers to a characteristic hyperpigmented appearance of the distal esophagus on endoscopy secondary to ischemic necrosis. AEN typically occurs in the setting of low-flow states leading to regional hypoperfusion and impaired intrinsic mucosal defense mechanisms, with concomitant corrosive injury from retrograde acidic contents. Here we present a case of AEN in the setting of sepsis and a newly diagnosed intrahepatic malignancy.
Case Description/Methods: A 74-year-old male with a past medical history of type II diabetes mellitus, coronary artery disease, GERD, and ulcerative colitis presented to the emergency department with complaint of nausea, vomiting, cough, shortness of breath, and abdominal pain. The patient was septic on arrival and started on empiric Zosyn and Azithromycin after a preliminary chest X-ray was consistent with pneumonia. He also underwent computed tomography (CT) scan of the abdomen that revealed a large heterogenous right hepatic mass suspicious for malignancy.
Gastroenterology was consulted and performed an esophagogastroduodenoscopy (EGD) that showed LA Grade D esophagitis with severe ulcers that were not bleeding, gastritis, multiple Forrest Class IIc duodenal ulcers, but no malignant appearing lesions.
The patient continued to have abdominal pain and new symptoms of reflux with early satiety during his hospitalization. To rule out gastric outlet obstruction, a repeat EGD was performed four days after the index endoscopy.
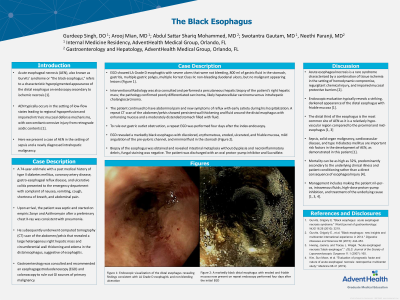
EGD revealed a markedly black esophagus with discolored, eroded, ulcerated, and friable mucosa, mild angulation of the pre-pyloric channel. Biopsy of the esophagus was obtained and revealed intestinal metaplasia without dysplasia and necroinflammatory debris. The patient was subsequently discharged with an oral proton-pump inhibitor and Sucralfate.
Discussion: Acute esophageal necrosis is a rare syndrome characterized by a combination of tissue ischemia in the setting of hemodynamic compromise, regurgitant chemical injury, and impaired mucosal protective barriers. Endoscopic evaluation typically reveals a striking, darkened appearance of the distal esophagus with friable mucosa.
Sepsis, solid organ malignancy, cardiovascular disease, and type II diabetes mellitus are important risk factors in the development of AEN, as demonstrated in this patient. Mortality can be as high as 32%, predominantly secondary to the underlying illness rather than a direct consequence of esophageal injury.

Disclosures:
Gurdeep Singh, DO, Arooj Mian, MD, Abdul Mohammed, MD, Swotantra Gautam, MD, Neethi Paranji, MD. P1924 - The Black Esophagus - A Case of Acute Esophageal Necrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
AdventHealth, Orlando, FL
Introduction: Acute esophageal necrosis (AEN), also known as “the black esophagus,” refers to a characteristic hyperpigmented appearance of the distal esophagus on endoscopy secondary to ischemic necrosis. AEN typically occurs in the setting of low-flow states leading to regional hypoperfusion and impaired intrinsic mucosal defense mechanisms, with concomitant corrosive injury from retrograde acidic contents. Here we present a case of AEN in the setting of sepsis and a newly diagnosed intrahepatic malignancy.
Case Description/Methods: A 74-year-old male with a past medical history of type II diabetes mellitus, coronary artery disease, GERD, and ulcerative colitis presented to the emergency department with complaint of nausea, vomiting, cough, shortness of breath, and abdominal pain. The patient was septic on arrival and started on empiric Zosyn and Azithromycin after a preliminary chest X-ray was consistent with pneumonia. He also underwent computed tomography (CT) scan of the abdomen that revealed a large heterogenous right hepatic mass suspicious for malignancy.
Gastroenterology was consulted and performed an esophagogastroduodenoscopy (EGD) that showed LA Grade D esophagitis with severe ulcers that were not bleeding, gastritis, multiple Forrest Class IIc duodenal ulcers, but no malignant appearing lesions.
The patient continued to have abdominal pain and new symptoms of reflux with early satiety during his hospitalization. To rule out gastric outlet obstruction, a repeat EGD was performed four days after the index endoscopy.
EGD revealed a markedly black esophagus with discolored, eroded, ulcerated, and friable mucosa, mild angulation of the pre-pyloric channel. Biopsy of the esophagus was obtained and revealed intestinal metaplasia without dysplasia and necroinflammatory debris. The patient was subsequently discharged with an oral proton-pump inhibitor and Sucralfate.
Discussion: Acute esophageal necrosis is a rare syndrome characterized by a combination of tissue ischemia in the setting of hemodynamic compromise, regurgitant chemical injury, and impaired mucosal protective barriers. Endoscopic evaluation typically reveals a striking, darkened appearance of the distal esophagus with friable mucosa.
Sepsis, solid organ malignancy, cardiovascular disease, and type II diabetes mellitus are important risk factors in the development of AEN, as demonstrated in this patient. Mortality can be as high as 32%, predominantly secondary to the underlying illness rather than a direct consequence of esophageal injury.

Figure: A: Endoscopic visualization of the distal esophagus revealing findings consistent with LA Grade D esophagitis and non-bleeding ulceration.
B: A markedly black distal esophagus with eroded and friable mucosa now present on repeat endoscopy performed four days after the initial EGD
B: A markedly black distal esophagus with eroded and friable mucosa now present on repeat endoscopy performed four days after the initial EGD
Disclosures:
Gurdeep Singh indicated no relevant financial relationships.
Arooj Mian indicated no relevant financial relationships.
Abdul Mohammed indicated no relevant financial relationships.
Swotantra Gautam indicated no relevant financial relationships.
Neethi Paranji indicated no relevant financial relationships.
Gurdeep Singh, DO, Arooj Mian, MD, Abdul Mohammed, MD, Swotantra Gautam, MD, Neethi Paranji, MD. P1924 - The Black Esophagus - A Case of Acute Esophageal Necrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
