Monday Poster Session
Category: Esophagus
P1926 - Double Trouble: Eosinophilic Esophagitis and Barrett’s Esophagus Overlap in a Young Female
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Megan Pranger, DO
Brooke Army Medical Center
Fort Sam Houston, TX
Presenting Author(s)
Megan Pranger, DO1, Howard Lee, MD1, Geoff Bader, MD2
1Brooke Army Medical Center, Fort Sam Houston, TX; 2Brooke Army Medical Center, San Antonio, TX
Introduction: Barrett’s esophagus (BE) and eosinophilic esophagitis (EoE) are well-described but distinct disorders of the esophagus. BE is recognized as a metaplastic change in the tubular esophagus due to gastroesophageal reflux disease (GERD), while EoE is an immune-mediated condition triggered by allergen exposure among genetically susceptible individuals causing eosinophil- predominate esophageal inflammation and fibrosis. EoE and BE are both common disorders, but their coexistence is rarely reported. We present a rare case of a young female with severe BE and EoE overlap.
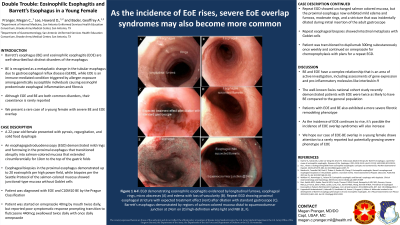
Case Description/Methods: A 22-year-old female presented with pyrosis, regurgitation, and solid food dysphagia. An esophagogastroduodenoscopy (EGD) demonstrated mild rings and furrowing in the proximal esophagus that transitioned abruptly into salmon-colored mucosa and extended 10cm circumferentially to the top of the gastric folds (Figure 1). Esophageal biopsies in the proximal esophagus demonstrated up to 20 eosinophils per high power field, while biopsies per the Seattle Protocol of the salmon-colored mucosa showed junctional-type mucosa without goblet cells. The patient was diagnosed with EoE and C10M10 BE by the Prague Classification. She was started on omeprazole 40 by mouth twice daily but reported poor symptomatic response prompting transition to fluticasone 440mcg swallowed twice daily and once daily omeprazole. Repeat EGD showed unchanged salmon colored mucosa, but the proximal esophagus exhibited mild edema and furrows, moderate rings, and a stricture that was incidentally dilated during initial insertion of the adult gastroscope (Figure 1). Repeat esophageal biopsies showed intestinal metaplasia with goblet cells. Patient was transitioned to dupilumab 300mg subcutaneously once weekly and continued omeprazole for chemoprophylaxis with plans for a repeat EGD.
Discussion: GERD and EoE have a complex relationship that is an area of active investigation, including assessments of gene expression and pro-inflammatory molecules like interleukin-9. The well-known Swiss national cohort study recently demonstrated patients with EoE were twice as likely to have BE compared to the general population; patients with EoE and BE also exhibited a more severe fibrotic remodeling phenotype. As the incidence of EoE rises, it’s possible the incidence of EoE overlap syndromes will also increase. We hope our case of EoE-BE overlap in a young female draws attention to a rarely reported but potentially growing severe phenotype of EoE.

Disclosures:
Megan Pranger, DO1, Howard Lee, MD1, Geoff Bader, MD2. P1926 - Double Trouble: Eosinophilic Esophagitis and Barrett’s Esophagus Overlap in a Young Female, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brooke Army Medical Center, Fort Sam Houston, TX; 2Brooke Army Medical Center, San Antonio, TX
Introduction: Barrett’s esophagus (BE) and eosinophilic esophagitis (EoE) are well-described but distinct disorders of the esophagus. BE is recognized as a metaplastic change in the tubular esophagus due to gastroesophageal reflux disease (GERD), while EoE is an immune-mediated condition triggered by allergen exposure among genetically susceptible individuals causing eosinophil- predominate esophageal inflammation and fibrosis. EoE and BE are both common disorders, but their coexistence is rarely reported. We present a rare case of a young female with severe BE and EoE overlap.
Case Description/Methods: A 22-year-old female presented with pyrosis, regurgitation, and solid food dysphagia. An esophagogastroduodenoscopy (EGD) demonstrated mild rings and furrowing in the proximal esophagus that transitioned abruptly into salmon-colored mucosa and extended 10cm circumferentially to the top of the gastric folds (Figure 1). Esophageal biopsies in the proximal esophagus demonstrated up to 20 eosinophils per high power field, while biopsies per the Seattle Protocol of the salmon-colored mucosa showed junctional-type mucosa without goblet cells. The patient was diagnosed with EoE and C10M10 BE by the Prague Classification. She was started on omeprazole 40 by mouth twice daily but reported poor symptomatic response prompting transition to fluticasone 440mcg swallowed twice daily and once daily omeprazole. Repeat EGD showed unchanged salmon colored mucosa, but the proximal esophagus exhibited mild edema and furrows, moderate rings, and a stricture that was incidentally dilated during initial insertion of the adult gastroscope (Figure 1). Repeat esophageal biopsies showed intestinal metaplasia with goblet cells. Patient was transitioned to dupilumab 300mg subcutaneously once weekly and continued omeprazole for chemoprophylaxis with plans for a repeat EGD.
Discussion: GERD and EoE have a complex relationship that is an area of active investigation, including assessments of gene expression and pro-inflammatory molecules like interleukin-9. The well-known Swiss national cohort study recently demonstrated patients with EoE were twice as likely to have BE compared to the general population; patients with EoE and BE also exhibited a more severe fibrotic remodeling phenotype. As the incidence of EoE rises, it’s possible the incidence of EoE overlap syndromes will also increase. We hope our case of EoE-BE overlap in a young female draws attention to a rarely reported but potentially growing severe phenotype of EoE.

Figure: Figure 1.
EGD demonstrating eosinophilic esophagitis evidenced by (A) longitudinal furrows, esophageal rings, micro abscesses, and (B) edema with loss of vascularity. Also notable for BE with C10M10 (C). Repeat EGD with proximal esophageal stricture and expected treatment effect (mucosal rent) after dilation with standard gastroscope. Barrett’s esophagus demonstrated by regions of salmon colored mucosa distal to squamocolumnar junction at 24cm (D) on high-definition white light (E) and (F) NBI.
EGD demonstrating eosinophilic esophagitis evidenced by (A) longitudinal furrows, esophageal rings, micro abscesses, and (B) edema with loss of vascularity. Also notable for BE with C10M10 (C). Repeat EGD with proximal esophageal stricture and expected treatment effect (mucosal rent) after dilation with standard gastroscope. Barrett’s esophagus demonstrated by regions of salmon colored mucosa distal to squamocolumnar junction at 24cm (D) on high-definition white light (E) and (F) NBI.
Disclosures:
Megan Pranger indicated no relevant financial relationships.
Howard Lee indicated no relevant financial relationships.
Geoff Bader indicated no relevant financial relationships.
Megan Pranger, DO1, Howard Lee, MD1, Geoff Bader, MD2. P1926 - Double Trouble: Eosinophilic Esophagitis and Barrett’s Esophagus Overlap in a Young Female, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
