Monday Poster Session
Category: Esophagus
P1927 - Brain Abscess Secondary to Streptococcus Intermedius Following an EGD with Biopsy in a Patient with Eosinophilic Esophagitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Nazli Begum Ozturk, MD
Beaumont Hospital
Royal Oak, MI
Presenting Author(s)
Nazli Begum Ozturk, MD, Tatjana Blazin, MD, Aparna Hariharan, MD, Naveen Reddy, MD
Beaumont Hospital, Royal Oak, MI
Introduction: Brain abscess is a rare complication of esophagogastroduodenoscopy (EGD) with few reported cases in the literature. In this case, we report a patient presenting with altered mental status, headache, and dysarthria due to brain abscess caused by Streptococcus intermedius (S. intermedius) shortly after an EGD with biopsy.
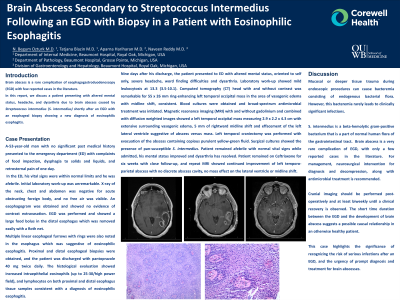
Case Description/Methods: A 53-year-old man with no significant past medical history presented to the emergency department (ED) with complaints of food impaction and retrosternal pain of one day. His vital signs were stable. An esophagogram was obtained and showed no evidence of contrast extravasation. EGD was performed and showed a large food bolus in the distal esophagus which was removed easily with an endoscopic retrieval device. Multiple linear esophageal furrows with rings were also noted which were suggestive of eosinophilic esophagitis. Proximal and distal esophageal biopsies were obtained and the patient was discharged with pantoprazole 40 mg twice daily. Histological evaluation reported a diagnosis of eosinophilic esophagitis. Nine days after his discharge, the patient presented to ED with altered mental status, severe headache and dysarthria. Laboratory work-up revealed mild leukocytosis of 13.3 (3.5-10.1). Computed tomography of the head was remarkable for 2.6 x 5.5 cm ring-enhancing left temporal occipital mass with midline shift, consistent with brain abscess. Blood cultures were obtained and broad-spectrum antimicrobial treatment was initiated. Following, magnetic resonance imaging (MRI) showed a left temporal occipital mass measuring 2.9 x 2.2 x 4.3 cm with extensive surrounding vasogenic edema and rightward midline shift. Left temporal craniectomy was performed with evacuation of the abscess. Surgical cultures showed the presence of pan-susceptible S. intermedius. The patient’s mental status and dysarthria has resolved while admitted. He remained on Ceftriaxone for six weeks and a repeat MRI showed continued improvement with no discrete abscess cavity or midline shift.
Discussion: Mucosal or deeper tissue trauma during EGD can cause bacteremia consisting of endogenous bacterial flora, however this bacteremia rarely leads to clinically significant infections. The short time duration between the EGD and the development of brain abscess in our case suggests a possible causal relationship. This case highlights the significance of recognizing the risk of serious infections after an EGD.

Disclosures:
Nazli Begum Ozturk, MD, Tatjana Blazin, MD, Aparna Hariharan, MD, Naveen Reddy, MD. P1927 - Brain Abscess Secondary to Streptococcus Intermedius Following an EGD with Biopsy in a Patient with Eosinophilic Esophagitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Beaumont Hospital, Royal Oak, MI
Introduction: Brain abscess is a rare complication of esophagogastroduodenoscopy (EGD) with few reported cases in the literature. In this case, we report a patient presenting with altered mental status, headache, and dysarthria due to brain abscess caused by Streptococcus intermedius (S. intermedius) shortly after an EGD with biopsy.
Case Description/Methods: A 53-year-old man with no significant past medical history presented to the emergency department (ED) with complaints of food impaction and retrosternal pain of one day. His vital signs were stable. An esophagogram was obtained and showed no evidence of contrast extravasation. EGD was performed and showed a large food bolus in the distal esophagus which was removed easily with an endoscopic retrieval device. Multiple linear esophageal furrows with rings were also noted which were suggestive of eosinophilic esophagitis. Proximal and distal esophageal biopsies were obtained and the patient was discharged with pantoprazole 40 mg twice daily. Histological evaluation reported a diagnosis of eosinophilic esophagitis. Nine days after his discharge, the patient presented to ED with altered mental status, severe headache and dysarthria. Laboratory work-up revealed mild leukocytosis of 13.3 (3.5-10.1). Computed tomography of the head was remarkable for 2.6 x 5.5 cm ring-enhancing left temporal occipital mass with midline shift, consistent with brain abscess. Blood cultures were obtained and broad-spectrum antimicrobial treatment was initiated. Following, magnetic resonance imaging (MRI) showed a left temporal occipital mass measuring 2.9 x 2.2 x 4.3 cm with extensive surrounding vasogenic edema and rightward midline shift. Left temporal craniectomy was performed with evacuation of the abscess. Surgical cultures showed the presence of pan-susceptible S. intermedius. The patient’s mental status and dysarthria has resolved while admitted. He remained on Ceftriaxone for six weeks and a repeat MRI showed continued improvement with no discrete abscess cavity or midline shift.
Discussion: Mucosal or deeper tissue trauma during EGD can cause bacteremia consisting of endogenous bacterial flora, however this bacteremia rarely leads to clinically significant infections. The short time duration between the EGD and the development of brain abscess in our case suggests a possible causal relationship. This case highlights the significance of recognizing the risk of serious infections after an EGD.

Figure: A: Brain abscess in left temporal occipital lobe on admission; B: Week 4 after craniectomy and parenteral IV antibiotic therapy
Disclosures:
Nazli Begum Ozturk indicated no relevant financial relationships.
Tatjana Blazin indicated no relevant financial relationships.
Aparna Hariharan indicated no relevant financial relationships.
Naveen Reddy indicated no relevant financial relationships.
Nazli Begum Ozturk, MD, Tatjana Blazin, MD, Aparna Hariharan, MD, Naveen Reddy, MD. P1927 - Brain Abscess Secondary to Streptococcus Intermedius Following an EGD with Biopsy in a Patient with Eosinophilic Esophagitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
