Monday Poster Session
Category: Functional Bowel Disease
P1941 - Effects of COVID-19 in Patients With Gastroparesis: An Analysis of Patients in the NIH Gastroparesis Registry
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- HP
Henry Parkman, MD
Temple University Hospital
Philadelphia, Andorra
Presenting Author(s)
Award: Outstanding Research Award in the Functional Bowel Disease Category
Award: Presidential Poster Award
Henry Parkman, MD1, Katherine Yates, 2, Richard McCallum, MD3, Kenneth Koch, MD4, Irene Sarosiek, MD5, Robert S. Bulat, MD6, Thomas Abell, MD7, Braden Kuo, MD8, Zubair Malik, MD1, Gianrico Farrugia, MD9, Bruno Chumpitazi, MD10, Robert Shulman, MD11, Laura Miriel, BS12, James Tonascia, PhD12, Frank Hamilton, MD13, Pankaj Pasricha, MD, MBBS14, Madhusudan Grover, MD9
1Temple University Hospital, Philadelphia, PA; 2Johns Hopkins, Baltimore, MD; 3TTUHSC, El Paso, TX; 4Wake Forest Universtiy, Wake Forest, NC; 5Texas Tech, El Paso, TX; 6Johns Hopkins Hospital, Baltimore, MD; 7University of Louisville, Louisville, LA; 8Massachusetts General Hospital, Boston, MA; 9Mayo Clinic, Rochester, MN; 10Baylor College of Medicine, Bruno, TX; 11Baylor College of Medicine, Houston, TX; 12Johns Hopkins University, Baltimore, MD; 13National Institutes of Health, Bethesda, MD; 14Mayo Clinic Arizona, Scottsdale, AZ
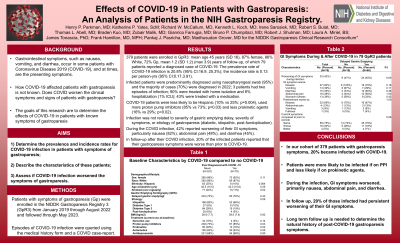
Introduction: Gastrointestinal symptoms occurred in some patients infected with Coronavirus Disease 2019 (COVID-19), and at times, were the presenting symptoms. How COVID-19 affected patients with gastroparesis that have impaired gastric function is not known. The aims of this study are to: 1) determine the prevalence incident rates for COVID-19 infection in patients with symptoms of gastroparesis; 2) describe the characteristics of these patients; 3) assess if COVID-19 infection worsened the symptoms of gastroparesis.
Methods: Methods: Patients with symptoms of gastroparesis (Gp) were enrolled in the NIDDK Gastroparesis Registry 3 (GpR3) from January 2019 through August 2022 and followed through May 2023. Episodes of COVID-19 infection were queried using the medical history form and a COVID case-report (CQ CRF).
Results: Results: 379 patients were enrolled in GpR3: mean age 45 years (SD 16), 87% female, 86% White, 72% Gp, mean 1.2 (SD 1.2) (max 3.9) years of follow-up, of which 79 patients reported a diagnosed case of COVID-19. The prevalence rate of COVID-19 infection is 20.8% (95% CI:16.9, 25.3%); the incidence rate is 0.13 per person-yrs (95% CI:0.17,3.91). Infected patients were predominantly diagnosed using nasopharyngeal swab (95%) and the majority of cases (70%) were diagnosed in 2022; 3 patients had 2 episodes of infection; 90% were treated with home isolation and 8% hospitalization (1% ICU); 43% were treated with a medication. COVID-19 patients were less likely to be Hispanic (10% vs 25%;p=0.004), used more proton pump inhibitors (85% vs 73%;p=0.03) and less prokinetic agents (16% vs 29%;p=0.02). Infection was not related to severity of gastric emptying delay, severity of symptoms, or etiology of gastroparesis (diabetic, idiopathic, postfundoplication). During the COVID infection, 42% reported worsening of their GI symptoms, particularly nausea (69%) and abdominal pain (13%). In follow-up after their COVID infection, 20% of the infected patients reported that their gastroparesis symptoms were worse than prior to COVID-19.
Discussion: Discussion: In our cohort of 379 patients with gastroparesis symptoms, 20% became infected with COVID-19. Patients were more likely to be infected if on PPI and less likely if on prokinetic agents. During the infection, GI symptoms worsened, primarily nausea and abdominal pain. In follow up, 20% of those infected had persistent worsening of their GI symptoms. Long term follow up is needed to determine the natural history of post COVID gastroparesis symptoms.
Disclosures:
Henry Parkman, MD1, Katherine Yates, 2, Richard McCallum, MD3, Kenneth Koch, MD4, Irene Sarosiek, MD5, Robert S. Bulat, MD6, Thomas Abell, MD7, Braden Kuo, MD8, Zubair Malik, MD1, Gianrico Farrugia, MD9, Bruno Chumpitazi, MD10, Robert Shulman, MD11, Laura Miriel, BS12, James Tonascia, PhD12, Frank Hamilton, MD13, Pankaj Pasricha, MD, MBBS14, Madhusudan Grover, MD9. P1941 - Effects of COVID-19 in Patients With Gastroparesis: An Analysis of Patients in the NIH Gastroparesis Registry, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Award: Presidential Poster Award
Henry Parkman, MD1, Katherine Yates, 2, Richard McCallum, MD3, Kenneth Koch, MD4, Irene Sarosiek, MD5, Robert S. Bulat, MD6, Thomas Abell, MD7, Braden Kuo, MD8, Zubair Malik, MD1, Gianrico Farrugia, MD9, Bruno Chumpitazi, MD10, Robert Shulman, MD11, Laura Miriel, BS12, James Tonascia, PhD12, Frank Hamilton, MD13, Pankaj Pasricha, MD, MBBS14, Madhusudan Grover, MD9
1Temple University Hospital, Philadelphia, PA; 2Johns Hopkins, Baltimore, MD; 3TTUHSC, El Paso, TX; 4Wake Forest Universtiy, Wake Forest, NC; 5Texas Tech, El Paso, TX; 6Johns Hopkins Hospital, Baltimore, MD; 7University of Louisville, Louisville, LA; 8Massachusetts General Hospital, Boston, MA; 9Mayo Clinic, Rochester, MN; 10Baylor College of Medicine, Bruno, TX; 11Baylor College of Medicine, Houston, TX; 12Johns Hopkins University, Baltimore, MD; 13National Institutes of Health, Bethesda, MD; 14Mayo Clinic Arizona, Scottsdale, AZ
Introduction: Gastrointestinal symptoms occurred in some patients infected with Coronavirus Disease 2019 (COVID-19), and at times, were the presenting symptoms. How COVID-19 affected patients with gastroparesis that have impaired gastric function is not known. The aims of this study are to: 1) determine the prevalence incident rates for COVID-19 infection in patients with symptoms of gastroparesis; 2) describe the characteristics of these patients; 3) assess if COVID-19 infection worsened the symptoms of gastroparesis.
Methods: Methods: Patients with symptoms of gastroparesis (Gp) were enrolled in the NIDDK Gastroparesis Registry 3 (GpR3) from January 2019 through August 2022 and followed through May 2023. Episodes of COVID-19 infection were queried using the medical history form and a COVID case-report (CQ CRF).
Results: Results: 379 patients were enrolled in GpR3: mean age 45 years (SD 16), 87% female, 86% White, 72% Gp, mean 1.2 (SD 1.2) (max 3.9) years of follow-up, of which 79 patients reported a diagnosed case of COVID-19. The prevalence rate of COVID-19 infection is 20.8% (95% CI:16.9, 25.3%); the incidence rate is 0.13 per person-yrs (95% CI:0.17,3.91). Infected patients were predominantly diagnosed using nasopharyngeal swab (95%) and the majority of cases (70%) were diagnosed in 2022; 3 patients had 2 episodes of infection; 90% were treated with home isolation and 8% hospitalization (1% ICU); 43% were treated with a medication. COVID-19 patients were less likely to be Hispanic (10% vs 25%;p=0.004), used more proton pump inhibitors (85% vs 73%;p=0.03) and less prokinetic agents (16% vs 29%;p=0.02). Infection was not related to severity of gastric emptying delay, severity of symptoms, or etiology of gastroparesis (diabetic, idiopathic, postfundoplication). During the COVID infection, 42% reported worsening of their GI symptoms, particularly nausea (69%) and abdominal pain (13%). In follow-up after their COVID infection, 20% of the infected patients reported that their gastroparesis symptoms were worse than prior to COVID-19.
Discussion: Discussion: In our cohort of 379 patients with gastroparesis symptoms, 20% became infected with COVID-19. Patients were more likely to be infected if on PPI and less likely if on prokinetic agents. During the infection, GI symptoms worsened, primarily nausea and abdominal pain. In follow up, 20% of those infected had persistent worsening of their GI symptoms. Long term follow up is needed to determine the natural history of post COVID gastroparesis symptoms.
Disclosures:
Henry Parkman indicated no relevant financial relationships.
Katherine Yates indicated no relevant financial relationships.
Richard McCallum: Evoke Pharma – Advisor or Review Panel Member.
Kenneth Koch indicated no relevant financial relationships.
Irene Sarosiek indicated no relevant financial relationships.
Robert Bulat indicated no relevant financial relationships.
Thomas Abell indicated no relevant financial relationships.
Braden Kuo indicated no relevant financial relationships.
Zubair Malik indicated no relevant financial relationships.
Gianrico Farrugia indicated no relevant financial relationships.
Bruno Chumpitazi indicated no relevant financial relationships.
Robert Shulman: Cairn Diagnostics – Grant/Research Support. Rome Foundation – Intellectual Property/Patents.
Laura Miriel indicated no relevant financial relationships.
James Tonascia indicated no relevant financial relationships.
Frank Hamilton indicated no relevant financial relationships.
Pankaj Pasricha: FoodMarble – Consultant. Neurogastrx – Consultant. Vanda – Consultant.
Madhusudan Grover indicated no relevant financial relationships.
Henry Parkman, MD1, Katherine Yates, 2, Richard McCallum, MD3, Kenneth Koch, MD4, Irene Sarosiek, MD5, Robert S. Bulat, MD6, Thomas Abell, MD7, Braden Kuo, MD8, Zubair Malik, MD1, Gianrico Farrugia, MD9, Bruno Chumpitazi, MD10, Robert Shulman, MD11, Laura Miriel, BS12, James Tonascia, PhD12, Frank Hamilton, MD13, Pankaj Pasricha, MD, MBBS14, Madhusudan Grover, MD9. P1941 - Effects of COVID-19 in Patients With Gastroparesis: An Analysis of Patients in the NIH Gastroparesis Registry, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

