Monday Poster Session
Category: Functional Bowel Disease
P1943 - A Minority of Patients in Need of Pelvic Floor Biofeedback Training (BFT) Actually Attend Scheduled Therapy Sessions
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Joseph A. Menand, MD
Mount Sinai Morningside-West
New York, NY
Presenting Author(s)
Joseph Menand, MD1, Robinderpal Sandhu, MD1, Yonatan Israel, BS2, Emma Reford, BA2, Ahmun Zafar, DO1, Kimberly Cavaliere, MD1, Priyanka Singh, MD1, Jean Saleh, MD3, Michael S.. Smith, MD, MBA2, Yuying Luo, MD4, Daniela Jodorkovsky, MD5
1Mount Sinai Morningside-West, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West, New York, NY; 4Center of GI Physiology and Motility at Mount Sinai West, New York, NY; 5Mount Sinai, New York, NY
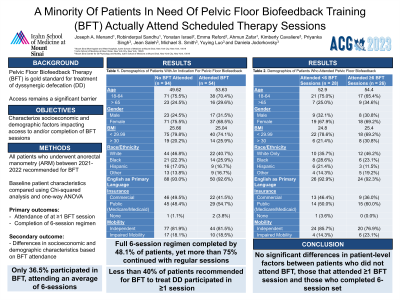
Introduction: Pelvic Floor Biofeedback Therapy (BFT) is the gold standard treatment for dyssynergic defecation (DD), but access to this intervention remains a significant barrier. We aim to characterize whether socioeconomic and demographic factors impact access to and completion of BFT sessions.
Methods: All patients who underwent anorectal manometry (ARM) between 2021-2022 at a single high-volume center with motility expertise were considered. Patients were included in the analysis if BFT was recommended based on ARM. Baseline patient characteristics were compared using Chi-squared analysis and one-way ANOVA. Primary outcomes were attendance of at least one BFT session and completion of a six-session regimen, if recommended. Secondary outcomes included differences in socioeconomic and demographic characteristics based on whether BFT was attended and completed.
Results: A total of 148 patients who underwent ARM were recommended for BFT (Table 1). Only 54 of 148 patients (36.5%) participated in BFT at the home site, attending an average of six sessions. A full six session regimen was completed by 48.1% of patients. There were no significant differences in patient-level factors between patients who attended BFT and those who did not. There were also no significant differences in patient-level factors between patients who attended at least 1-5 BFT sessions compared to those who completed a minimum set of six sessions.
Discussion: In this cohort, less than 40% of patients recommended for BFT to treat DD participated in at least one session. Additionally, a minority of those who attended at least one session completed the standard set of six visits. Interestingly, more than 75% of those who completed six sessions continued with regular BFT. There were no socio-demographic factors that were found to impact BFT attendance. Study limitations include the quality and availability of retrospectively collected data. This study should prompt further prospective research to qualitatively assess patient and healthcare system barriers to BFT attendance and completion, to develop patient-centered interventions to improve show rates.
Disclosures:
Joseph Menand, MD1, Robinderpal Sandhu, MD1, Yonatan Israel, BS2, Emma Reford, BA2, Ahmun Zafar, DO1, Kimberly Cavaliere, MD1, Priyanka Singh, MD1, Jean Saleh, MD3, Michael S.. Smith, MD, MBA2, Yuying Luo, MD4, Daniela Jodorkovsky, MD5. P1943 - A Minority of Patients in Need of Pelvic Floor Biofeedback Training (BFT) Actually Attend Scheduled Therapy Sessions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mount Sinai Morningside-West, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West, New York, NY; 4Center of GI Physiology and Motility at Mount Sinai West, New York, NY; 5Mount Sinai, New York, NY
Introduction: Pelvic Floor Biofeedback Therapy (BFT) is the gold standard treatment for dyssynergic defecation (DD), but access to this intervention remains a significant barrier. We aim to characterize whether socioeconomic and demographic factors impact access to and completion of BFT sessions.
Methods: All patients who underwent anorectal manometry (ARM) between 2021-2022 at a single high-volume center with motility expertise were considered. Patients were included in the analysis if BFT was recommended based on ARM. Baseline patient characteristics were compared using Chi-squared analysis and one-way ANOVA. Primary outcomes were attendance of at least one BFT session and completion of a six-session regimen, if recommended. Secondary outcomes included differences in socioeconomic and demographic characteristics based on whether BFT was attended and completed.
Results: A total of 148 patients who underwent ARM were recommended for BFT (Table 1). Only 54 of 148 patients (36.5%) participated in BFT at the home site, attending an average of six sessions. A full six session regimen was completed by 48.1% of patients. There were no significant differences in patient-level factors between patients who attended BFT and those who did not. There were also no significant differences in patient-level factors between patients who attended at least 1-5 BFT sessions compared to those who completed a minimum set of six sessions.
Discussion: In this cohort, less than 40% of patients recommended for BFT to treat DD participated in at least one session. Additionally, a minority of those who attended at least one session completed the standard set of six visits. Interestingly, more than 75% of those who completed six sessions continued with regular BFT. There were no socio-demographic factors that were found to impact BFT attendance. Study limitations include the quality and availability of retrospectively collected data. This study should prompt further prospective research to qualitatively assess patient and healthcare system barriers to BFT attendance and completion, to develop patient-centered interventions to improve show rates.
Disclosures:
Joseph Menand indicated no relevant financial relationships.
Robinderpal Sandhu indicated no relevant financial relationships.
Yonatan Israel indicated no relevant financial relationships.
Emma Reford indicated no relevant financial relationships.
Ahmun Zafar indicated no relevant financial relationships.
Kimberly Cavaliere indicated no relevant financial relationships.
Priyanka Singh indicated no relevant financial relationships.
Jean Saleh indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Consultant. Provation Medical – Consultant. Steris Endoscopy – Consultant.
Yuying Luo indicated no relevant financial relationships.
Daniela Jodorkovsky: ATMO Biosciences – Consultant.
Joseph Menand, MD1, Robinderpal Sandhu, MD1, Yonatan Israel, BS2, Emma Reford, BA2, Ahmun Zafar, DO1, Kimberly Cavaliere, MD1, Priyanka Singh, MD1, Jean Saleh, MD3, Michael S.. Smith, MD, MBA2, Yuying Luo, MD4, Daniela Jodorkovsky, MD5. P1943 - A Minority of Patients in Need of Pelvic Floor Biofeedback Training (BFT) Actually Attend Scheduled Therapy Sessions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
