Monday Poster Session
Category: Functional Bowel Disease
P1944 - Patient-Level Factors Do Not Impact Therapeutic Escalation in Chronic Constipation
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Ahmun Zafar, DO
Mount Sinai Morningside-West
New York, NY
Presenting Author(s)
Ahmun Zafar, DO1, Joseph Menand, MD1, Robinderpal Sandhu, MD1, Yonatan Israel, BS2, Emma Reford, BA2, Kimberly Cavaliere, MD1, Priyanka Singh, MD1, Jean Saleh, MD3, Michael S.. Smith, MD, MBA2, Daniela Jodorkovsky, MD4, Yuying Luo, MD5
1Mount Sinai Morningside-West, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West, New York, NY; 4Mount Sinai, New York, NY; 5Center of GI Physiology and Motility at Mount Sinai West, New York, NY
Introduction: Prior to undergoing anorectal manometry (ARM) for chronic constipation, treatment guidelines recommend lifestyle modifications, followed by over the counter (OTC) medications and then prescription (Rx) medications. It is unclear if there are patient-level factors as to who is escalated on therapies and if there are higher rates of dyssynergic defecation (DD) in the patients who require Rx laxatives.
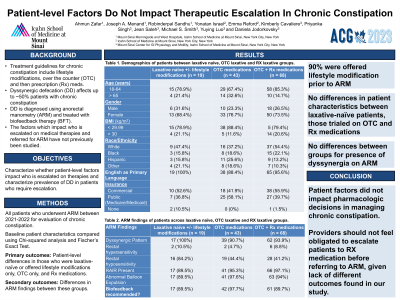
Methods: A retrospective study of all consecutive patients who underwent ARM between 2021-2022 at one tertiary center with motility expertise was performed. Baseline patient characteristics (age, race, BMI, English as a primary language and insurance status) were compared with Chi-squared and Fischer’s Exact Test. Our primary outcomes were patient-level differences in those who were laxative-naïve or offered lifestyle modifications only, OTC only, and Rx medications. Secondary analysis included differences in ARM findings between these groups.
Results: We included 130 patients with documented medication use prior to ARM for chronic constipation or difficulty evacuating. Of this cohort, 90% were offered some form of lifestyle modification prior to ARM, specifically 80.8% were recommended fiber. There were no significant differences in patient characteristics between laxative-naïve patients (n=19), those trialed on OTC (n=43) and Rx medications (n=68) (Table 1). There were no differences between the groups for presence of dyssynergia on ARM; however, the laxative-naïve group had significantly higher rates of rectal hyposensitivity (p = .003) compared to the OTC and Rx group.
Discussion: In this cohort a majority of all patient groups had been offered lifestyle modification. Most patients had been escalated to Rx laxatives for chronic constipation prior to diagnosis of DD and recommendation for BFT. Reassuringly, our study did not find any patient-level differences between patients based on whether they had been on OTC or Rx treatments, suggesting that socioeconomic level differences do not guide pharmacologic decisions in managing chronic constipation. Furthermore, as there were no differences in the presence of dyssynergia on ARM between laxative-naive patients and those on Rx laxatives, if there is clinical suspicion for an evacuation disorder, perhaps providers should not feel obligated to escalate patients to Rx laxatives before referring for ARM. Limitations include the relatively small sample size and the inherent limitations in retrospective data.
Disclosures:
Ahmun Zafar, DO1, Joseph Menand, MD1, Robinderpal Sandhu, MD1, Yonatan Israel, BS2, Emma Reford, BA2, Kimberly Cavaliere, MD1, Priyanka Singh, MD1, Jean Saleh, MD3, Michael S.. Smith, MD, MBA2, Daniela Jodorkovsky, MD4, Yuying Luo, MD5. P1944 - Patient-Level Factors Do Not Impact Therapeutic Escalation in Chronic Constipation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mount Sinai Morningside-West, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West, New York, NY; 4Mount Sinai, New York, NY; 5Center of GI Physiology and Motility at Mount Sinai West, New York, NY
Introduction: Prior to undergoing anorectal manometry (ARM) for chronic constipation, treatment guidelines recommend lifestyle modifications, followed by over the counter (OTC) medications and then prescription (Rx) medications. It is unclear if there are patient-level factors as to who is escalated on therapies and if there are higher rates of dyssynergic defecation (DD) in the patients who require Rx laxatives.
Methods: A retrospective study of all consecutive patients who underwent ARM between 2021-2022 at one tertiary center with motility expertise was performed. Baseline patient characteristics (age, race, BMI, English as a primary language and insurance status) were compared with Chi-squared and Fischer’s Exact Test. Our primary outcomes were patient-level differences in those who were laxative-naïve or offered lifestyle modifications only, OTC only, and Rx medications. Secondary analysis included differences in ARM findings between these groups.
Results: We included 130 patients with documented medication use prior to ARM for chronic constipation or difficulty evacuating. Of this cohort, 90% were offered some form of lifestyle modification prior to ARM, specifically 80.8% were recommended fiber. There were no significant differences in patient characteristics between laxative-naïve patients (n=19), those trialed on OTC (n=43) and Rx medications (n=68) (Table 1). There were no differences between the groups for presence of dyssynergia on ARM; however, the laxative-naïve group had significantly higher rates of rectal hyposensitivity (p = .003) compared to the OTC and Rx group.
Discussion: In this cohort a majority of all patient groups had been offered lifestyle modification. Most patients had been escalated to Rx laxatives for chronic constipation prior to diagnosis of DD and recommendation for BFT. Reassuringly, our study did not find any patient-level differences between patients based on whether they had been on OTC or Rx treatments, suggesting that socioeconomic level differences do not guide pharmacologic decisions in managing chronic constipation. Furthermore, as there were no differences in the presence of dyssynergia on ARM between laxative-naive patients and those on Rx laxatives, if there is clinical suspicion for an evacuation disorder, perhaps providers should not feel obligated to escalate patients to Rx laxatives before referring for ARM. Limitations include the relatively small sample size and the inherent limitations in retrospective data.
Disclosures:
Ahmun Zafar indicated no relevant financial relationships.
Joseph Menand indicated no relevant financial relationships.
Robinderpal Sandhu indicated no relevant financial relationships.
Yonatan Israel indicated no relevant financial relationships.
Emma Reford indicated no relevant financial relationships.
Kimberly Cavaliere indicated no relevant financial relationships.
Priyanka Singh indicated no relevant financial relationships.
Jean Saleh indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Consultant. Provation Medical – Consultant. Steris Endoscopy – Consultant.
Daniela Jodorkovsky indicated no relevant financial relationships.
Yuying Luo indicated no relevant financial relationships.
Ahmun Zafar, DO1, Joseph Menand, MD1, Robinderpal Sandhu, MD1, Yonatan Israel, BS2, Emma Reford, BA2, Kimberly Cavaliere, MD1, Priyanka Singh, MD1, Jean Saleh, MD3, Michael S.. Smith, MD, MBA2, Daniela Jodorkovsky, MD4, Yuying Luo, MD5. P1944 - Patient-Level Factors Do Not Impact Therapeutic Escalation in Chronic Constipation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
