Monday Poster Session
Category: Functional Bowel Disease
P1954 - Long-Term, Non-Invasive, Objective Stool Monitoring Using a Novel Smart Toilet: A Feasibility Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sonia Grego, PhD
Coprata
Durham, NC
Presenting Author(s)
Sonia Grego, PhD1, Jin Zhou, MS2, Jose R. Ruiz, MD, MPH3, Kyle Lafata, PhD2, Brian Hawkins, PhD2, Yuying Luo, MD4
1Coprata, Durham, NC; 2Duke University, Durham, NC; 3University of Pennsylvania, Philadelphia, PA; 4Center of GI Physiology and Motility at Mount Sinai West, New York, NY
Introduction: Major discrepancies have been reported between patients’ self-report and objective features of stool consistency, a clinical marker used for gastroenterologists’ (GI) assessment of constipation or diarrhea. To achieve hassle-free and objective monitoring of a patient’s bowel movements (BM) over a prolonged period, we developed a novel image-capture system with the Smart Toilet. The aim of the current study is to demonstrate feasibility of image data collection and analysis by the Smart Toilet in healthy controls.
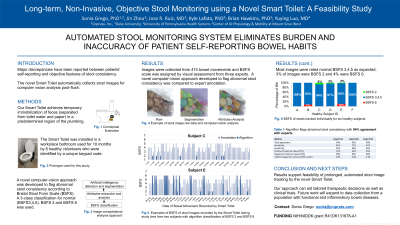
Methods: Our Smart Toilet integrates a conventional toilet bowl with an engineered portal that achieves temporary immobilization of feces (separated from toilet water and paper) in a predetermined region of the plumbing with a camera connected to a microcomputer which transmits images through Wi-Fi to a database. The Smart Toilet was installed in a workplace bathroom used by healthy volunteers identified by a unique keypad code. Images were annotated by two GI specialists according to the Bristol Stool Form Scale (BSFS). A novel computer-vision approach was developed for image analysis automation that systematically quantifies stool morphological attributes such as lumps after image segmentation in order to flag abnormal stool consistency.
Results: We collected images from 377 bowel movements from 6 healthy subjects over 8 months. Consistency was largely normal, with BSFS3/4/5 being observed in 17/44/30% of the images, demonstrating validity of using this toilet to track BM. BSFS 2 (2% of the stools) and BSFS 6 (6%) were also observed, demonstrating that the toilet captures abnormal BMs. BSFS scale was assigned by visual assessment according to morphological features such as lumps and cracks. Using a deterministic computer-vision approach, we developed an algorithm that flags abnormal stool consistency (BSFS 2 and 6) achieving 97% NPV (negative predictive value) for normal consistency and 50% PPV (positive predictive value).
Discussion: These results support feasibility of prolonged, non-invasive stool image tracking by the novel Smart Toilet and automated analysis. Future work will expand to data collection from a population with functional and inflammatory bowel diseases. This technology installed in the home has the potential to monitor and validate reports of diarrhea or constipation in patients and response to therapies.

Disclosures:
Sonia Grego, PhD1, Jin Zhou, MS2, Jose R. Ruiz, MD, MPH3, Kyle Lafata, PhD2, Brian Hawkins, PhD2, Yuying Luo, MD4. P1954 - Long-Term, Non-Invasive, Objective Stool Monitoring Using a Novel Smart Toilet: A Feasibility Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Coprata, Durham, NC; 2Duke University, Durham, NC; 3University of Pennsylvania, Philadelphia, PA; 4Center of GI Physiology and Motility at Mount Sinai West, New York, NY
Introduction: Major discrepancies have been reported between patients’ self-report and objective features of stool consistency, a clinical marker used for gastroenterologists’ (GI) assessment of constipation or diarrhea. To achieve hassle-free and objective monitoring of a patient’s bowel movements (BM) over a prolonged period, we developed a novel image-capture system with the Smart Toilet. The aim of the current study is to demonstrate feasibility of image data collection and analysis by the Smart Toilet in healthy controls.
Methods: Our Smart Toilet integrates a conventional toilet bowl with an engineered portal that achieves temporary immobilization of feces (separated from toilet water and paper) in a predetermined region of the plumbing with a camera connected to a microcomputer which transmits images through Wi-Fi to a database. The Smart Toilet was installed in a workplace bathroom used by healthy volunteers identified by a unique keypad code. Images were annotated by two GI specialists according to the Bristol Stool Form Scale (BSFS). A novel computer-vision approach was developed for image analysis automation that systematically quantifies stool morphological attributes such as lumps after image segmentation in order to flag abnormal stool consistency.
Results: We collected images from 377 bowel movements from 6 healthy subjects over 8 months. Consistency was largely normal, with BSFS3/4/5 being observed in 17/44/30% of the images, demonstrating validity of using this toilet to track BM. BSFS 2 (2% of the stools) and BSFS 6 (6%) were also observed, demonstrating that the toilet captures abnormal BMs. BSFS scale was assigned by visual assessment according to morphological features such as lumps and cracks. Using a deterministic computer-vision approach, we developed an algorithm that flags abnormal stool consistency (BSFS 2 and 6) achieving 97% NPV (negative predictive value) for normal consistency and 50% PPV (positive predictive value).
Discussion: These results support feasibility of prolonged, non-invasive stool image tracking by the novel Smart Toilet and automated analysis. Future work will expand to data collection from a population with functional and inflammatory bowel diseases. This technology installed in the home has the potential to monitor and validate reports of diarrhea or constipation in patients and response to therapies.

Figure: (A) Conceptual illustration of the Smart Toilet equipped with stool imaging capability. (B) Example of stool image from the Smart Toilet. (C) Computational segmentation of image B illustrates morphological features leveraged to detect abnormal BSFS. (D) Illustrative plot of BSFS of stool images recorded over a month period from multiple users of the Smart Toilet; BSFS annotation by a gastroenterologist and by algorithm detecting abnormal BSFS 2 and 6. (E). BSFS of stools tracked individually for six healthy subjects (a-f) over 8 months
Disclosures:
Sonia Grego: Coprata – Advisory Committee/Board Member, Grant/Research Support, Intellectual Property/Patents, Stock-privately held company.
Jin Zhou indicated no relevant financial relationships.
Jose Ruiz: Coprata – Consultant, Stock Options.
Kyle Lafata indicated no relevant financial relationships.
Brian Hawkins: Coprata – Intellectual Property/Patents.
Yuying Luo indicated no relevant financial relationships.
Sonia Grego, PhD1, Jin Zhou, MS2, Jose R. Ruiz, MD, MPH3, Kyle Lafata, PhD2, Brian Hawkins, PhD2, Yuying Luo, MD4. P1954 - Long-Term, Non-Invasive, Objective Stool Monitoring Using a Novel Smart Toilet: A Feasibility Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
