Monday Poster Session
Category: General Endoscopy
P1979 - United States Inpatient Gastrointestinal Procedures During the COVID-19 Pandemic – A Systemic Analysis of a Nationwide Sample
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Yuting Huang, MBBS, PhD
Mayo Clinic Florida
Jacksonville, FL
Presenting Author(s)
Yuting Huang, MBBS, PhD1, Yichen Wang, MD, MSc2, Dilhana Badurdeen, MD1
1Mayo Clinic Florida, Jacksonville, FL; 2Mercy Internal Medicine Service, Trinity Health of New England, Springfield, MA
Introduction: The COVID-19 pandemic resulted in a 17% increase in mortality and a 1.8-year decline in life expectancy across the United States (US) in 2020. Given the impact on public health and in-patient hospital procedure volume, we aimed to evaluate the impact of the COVID-19 pandemic on the volume of in-patient gastrointestinal (GI) procedures.
Methods: This was a retrospective cross-sectional epidemiologic study of hospitalizations with an in-patient GI procedure at acute care hospitals across the US from Jan 2019 to Dec 2020. The National Inpatient Sample (NIS) database was searched for categorical codes of GI procedures using the Healthcare Cost and Utilization Project (HCUP) designed Clinical Classifications Software Refined (CCSR) tool. The CCSR aggregates ICD-10-PCS codes into clinically meaningful categories. The NIS database was cross referenced for data quality using HCUP state inpatient databases.
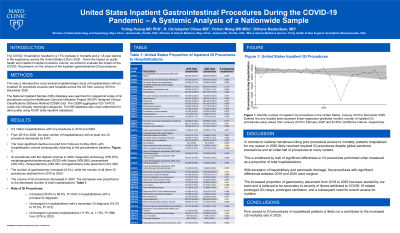
Results: There were 5.5 million and 5.1 million hospitalizations with GI procedures in 2019 and 2020, respectively. From 2019 to 2020, the total number of hospitalizations with at least one GI procedure decreased by 8.6%. The most significant decline occurred from Feb to May 2020, with hospitalization volume subsequently returning to pre-pandemic baseline (Figure). GI procedures with the highest volumes in 2020 were diagnostic endoscopy (576,915), esophagogastroduodenoscopy (EGD) with biopsy (508,595), paracentesis (320,160), cholecystectomy (283,320), and gastrostomy tube placement (241,320). The number of gastrostomies increased (8.3%), while the number of all other GI procedures declined from 2019 to 2020.
The volume of GI procedures decreased in 2020, and the decrease was proportional to the decreased number of total hospitalizations (Table). In fact, the rate of GI procedures increased (55.6% to 56.4%, P =.003) in hospitalizations with a principal GI diagnosis, remained unchanged in hospitalizations with a secondary GI diagnosis (18.2% to 18.3%, P =.512), and unchanged in general hospitalizations (11.9% vs. 11.9%, P =.588) from 2019 to 2020.
Discussion: In contrast to national narratives linking poor procedural access to mortality, patients hospitalized for any reason in 2020 likely received required GI procedures despite global pandemic precautions and an initial halt of procedures at many centers. Therefore, poor access to GI procedures in hospitalized patients is likely not a contributor to the increased US mortality rate in 2020.

Disclosures:
Yuting Huang, MBBS, PhD1, Yichen Wang, MD, MSc2, Dilhana Badurdeen, MD1. P1979 - United States Inpatient Gastrointestinal Procedures During the COVID-19 Pandemic – A Systemic Analysis of a Nationwide Sample, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mayo Clinic Florida, Jacksonville, FL; 2Mercy Internal Medicine Service, Trinity Health of New England, Springfield, MA
Introduction: The COVID-19 pandemic resulted in a 17% increase in mortality and a 1.8-year decline in life expectancy across the United States (US) in 2020. Given the impact on public health and in-patient hospital procedure volume, we aimed to evaluate the impact of the COVID-19 pandemic on the volume of in-patient gastrointestinal (GI) procedures.
Methods: This was a retrospective cross-sectional epidemiologic study of hospitalizations with an in-patient GI procedure at acute care hospitals across the US from Jan 2019 to Dec 2020. The National Inpatient Sample (NIS) database was searched for categorical codes of GI procedures using the Healthcare Cost and Utilization Project (HCUP) designed Clinical Classifications Software Refined (CCSR) tool. The CCSR aggregates ICD-10-PCS codes into clinically meaningful categories. The NIS database was cross referenced for data quality using HCUP state inpatient databases.
Results: There were 5.5 million and 5.1 million hospitalizations with GI procedures in 2019 and 2020, respectively. From 2019 to 2020, the total number of hospitalizations with at least one GI procedure decreased by 8.6%. The most significant decline occurred from Feb to May 2020, with hospitalization volume subsequently returning to pre-pandemic baseline (Figure). GI procedures with the highest volumes in 2020 were diagnostic endoscopy (576,915), esophagogastroduodenoscopy (EGD) with biopsy (508,595), paracentesis (320,160), cholecystectomy (283,320), and gastrostomy tube placement (241,320). The number of gastrostomies increased (8.3%), while the number of all other GI procedures declined from 2019 to 2020.
The volume of GI procedures decreased in 2020, and the decrease was proportional to the decreased number of total hospitalizations (Table). In fact, the rate of GI procedures increased (55.6% to 56.4%, P =.003) in hospitalizations with a principal GI diagnosis, remained unchanged in hospitalizations with a secondary GI diagnosis (18.2% to 18.3%, P =.512), and unchanged in general hospitalizations (11.9% vs. 11.9%, P =.588) from 2019 to 2020.
Discussion: In contrast to national narratives linking poor procedural access to mortality, patients hospitalized for any reason in 2020 likely received required GI procedures despite global pandemic precautions and an initial halt of procedures at many centers. Therefore, poor access to GI procedures in hospitalized patients is likely not a contributor to the increased US mortality rate in 2020.

Figure: Monthly number of inpatient GI procedures in the United States, January 2019 to December 2020. Dash line and shaded area represent linear-regresssion-predicted monthly number of inpatient GI procedures using values from January 2019 to February 2020 and its 95% confidence interval, respectively.
Disclosures:
Yuting Huang indicated no relevant financial relationships.
Yichen Wang indicated no relevant financial relationships.
Dilhana Badurdeen indicated no relevant financial relationships.
Yuting Huang, MBBS, PhD1, Yichen Wang, MD, MSc2, Dilhana Badurdeen, MD1. P1979 - United States Inpatient Gastrointestinal Procedures During the COVID-19 Pandemic – A Systemic Analysis of a Nationwide Sample, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
