Monday Poster Session
Category: General Endoscopy
P1992 - Endoscopic Management of Weight Regain Due to Staple-Line Dehiscence in a Patient With a Vertical Banded Gastroplasty
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Shae Patel, DO
Loma Linda University Health
Placentia, CA
Presenting Author(s)
Shae Patel, DO1, Devika Gandhi, MD2, Wasseem Skef, MD3
1Loma Linda University Health, Placentia, CA; 2Loma Linda University, Loma Linda, CA; 3Baylor College of Medicine, Houston, TX
Introduction: Vertical banded gastroplasty (VBG) is a restrictive surgical procedure for weight loss that was popular in the 1980s and 1990s. In this procedure, a band and staples are used to create a small gastric pouch. A common complication is staple-line insufficiency which can lead to weight regain. Weight regain after VBG is typically treated with conversion to Roux-en-Y gastric bypass (RYGB) – albeit this is associated with high morbidity. Herein, we present a case of weight regain due to staple-line dehiscence of a vertical banded gastroplasty that was managed with endoscopic suturing.
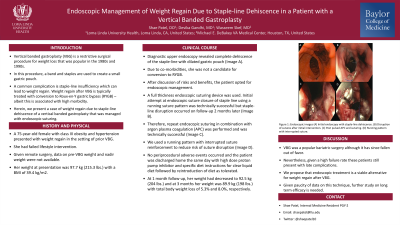
Case Description/Methods: A 75-year-old female with class III obesity and hypertension presented with weight regain in the setting of prior VBG. She had failed lifestyle intervention. Given remote surgery, data on pre-VBG weight and nadir weight were not available. Her weight at presentation was 97.7 kg (215.3 lbs.) with a BMI of 39.4 kg/m2. Diagnostic upper endoscopy revealed complete dehiscence of the staple-line with dilated gastric pouch (Image A). Due to co-morbidities, she was not a candidate for conversion to RYGB. After discussion of risks and benefits, the patient opted for endoscopic management. A full thickness endoscopic suturing device was used. Initial attempt at endoscopic suture closure of staple line using a running suture pattern was technically successful but staple-line disruption occurred on follow-up 2 months later (Image B). Therefore, repeat endoscopic suturing in combination with argon plasma coagulation (APC) was performed and was technically successful (Image C). We used a running pattern with interrupted suture reinforcement to reduce risk of suture disruption (Image D). No periprocedural adverse events occurred and the patient was discharged home the same day with high dose proton pump inhibitor and specific diet instructions for clear liquid diet followed by reintroduction of diet as tolerated. At 1 month follow-up, her weight had decreased to 92.5 kg (204 lbs.) and at 3 months her weight was 89.9 kg (198 lbs.) with total body weight loss of 5.3% and 8.0%, respectively.
Discussion: VBG was a popular bariatric surgery although it has since fallen out of favor. Nevertheless, given a high failure rate these patients still present with late complications. We propose that endoscopic treatment is a viable alternative for weight regain after VBG. Given paucity of data on this technique, further study on long term efficacy is needed.

Disclosures:
Shae Patel, DO1, Devika Gandhi, MD2, Wasseem Skef, MD3. P1992 - Endoscopic Management of Weight Regain Due to Staple-Line Dehiscence in a Patient With a Vertical Banded Gastroplasty, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Loma Linda University Health, Placentia, CA; 2Loma Linda University, Loma Linda, CA; 3Baylor College of Medicine, Houston, TX
Introduction: Vertical banded gastroplasty (VBG) is a restrictive surgical procedure for weight loss that was popular in the 1980s and 1990s. In this procedure, a band and staples are used to create a small gastric pouch. A common complication is staple-line insufficiency which can lead to weight regain. Weight regain after VBG is typically treated with conversion to Roux-en-Y gastric bypass (RYGB) – albeit this is associated with high morbidity. Herein, we present a case of weight regain due to staple-line dehiscence of a vertical banded gastroplasty that was managed with endoscopic suturing.
Case Description/Methods: A 75-year-old female with class III obesity and hypertension presented with weight regain in the setting of prior VBG. She had failed lifestyle intervention. Given remote surgery, data on pre-VBG weight and nadir weight were not available. Her weight at presentation was 97.7 kg (215.3 lbs.) with a BMI of 39.4 kg/m2. Diagnostic upper endoscopy revealed complete dehiscence of the staple-line with dilated gastric pouch (Image A). Due to co-morbidities, she was not a candidate for conversion to RYGB. After discussion of risks and benefits, the patient opted for endoscopic management. A full thickness endoscopic suturing device was used. Initial attempt at endoscopic suture closure of staple line using a running suture pattern was technically successful but staple-line disruption occurred on follow-up 2 months later (Image B). Therefore, repeat endoscopic suturing in combination with argon plasma coagulation (APC) was performed and was technically successful (Image C). We used a running pattern with interrupted suture reinforcement to reduce risk of suture disruption (Image D). No periprocedural adverse events occurred and the patient was discharged home the same day with high dose proton pump inhibitor and specific diet instructions for clear liquid diet followed by reintroduction of diet as tolerated. At 1 month follow-up, her weight had decreased to 92.5 kg (204 lbs.) and at 3 months her weight was 89.9 kg (198 lbs.) with total body weight loss of 5.3% and 8.0%, respectively.
Discussion: VBG was a popular bariatric surgery although it has since fallen out of favor. Nevertheless, given a high failure rate these patients still present with late complications. We propose that endoscopic treatment is a viable alternative for weight regain after VBG. Given paucity of data on this technique, further study on long term efficacy is needed.

Figure: Figure 1: Endoscopic images (A) Initial endoscopy with staple-line dehiscence. (B) Disruption of sutures after initial intervention. (C) Post pulsed APC and suturing. (D) Running pattern with interrupted suture.
Disclosures:
Shae Patel indicated no relevant financial relationships.
Devika Gandhi indicated no relevant financial relationships.
Wasseem Skef: GE Healthcare – Stock-publicly held company(excluding mutual/index funds).
Shae Patel, DO1, Devika Gandhi, MD2, Wasseem Skef, MD3. P1992 - Endoscopic Management of Weight Regain Due to Staple-Line Dehiscence in a Patient With a Vertical Banded Gastroplasty, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
