Monday Poster Session
Category: General Endoscopy
P1994 - Bleeding Dieulafoy’s Lesion: Refractory to All Endoscopic Measures
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Steven Kessler, BS
Oakland University William Beaumont School of Medicine
Rochester, MI
Presenting Author(s)
Steven Kessler, BS1, Prekchha Jha, MBBS2, Mihaela Batke, MD2
1Oakland University William Beaumont School of Medicine, Rochester, MI; 2Corewell Health, Royal Oak, MI
Introduction: Dieulafoy’s lesion is a developmental vascular malformation often located in the stomach. One third can have extra gastric location, frequently the duodenum. These account for 1-2% of acute gastrointestinal (GI) bleeding. Prior to advancement in endoscopic techniques, mortality was as high as 80%. Endoscopic therapy success rate is reported to be 90%. We present a case of a bleeding duodenal Dieulafoy’s lesion refractory to endoscopic hemostasis.
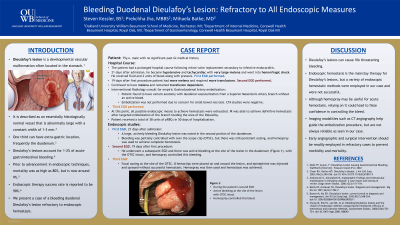
Case Description/Methods: 75-year-old man with a prolonged hospital course after mitral valve replacement for infective endocarditis developed large melanotic stools at day 21 of admission. Esophagogastroduodenoscopy (EGD) showed a large bleeding Dieulafoy’s lesion in the second portion of the duodenum. Hemostasis was achieved with over the scope clip (OTSC). He continued to have low volume melena and required transfusion of 1-2 units of packed red blood cells (pRBC) every 1-2 days. EGD 2 weeks later showed active bleeding around edges of the OTSC, and was controlled by hemospray application. He continued to have melena and remained transfusion dependent. Interventional Radiology (IR) was consulted for empiric Gastro Duodenal Artery (GDA) embolization. Unfortunately, he had variant anatomy with duodenal vascularization from a Superior Mesenteric Artery (SMA) branch without active bleed. Empiric embolization was not performed due to concern of acute small bowel necrosis. Computed Tomography Angiography studies were negative. A third EGD revealed continued bleeding at the site of the OTSC. Attempts to attain hemostasis were made with 8 hemoclips and epinephrine injection but were unsuccessful. Temporary hemostasis was achieved with hemospray. At this point, all possible endoscopic means to achieve hemostasis were exhausted. IR was able to achieve definitive hemostasis after targeted embolization of the branch feeding the area of the Dieulafoy. Patient received a total of 38 units of pRBC in 50 days of hospitalization.
Discussion: Dieulafoy’s lesions can cause life threatening bleeding. Endoscopic hemostasis is the mainstay therapy but this is not always successful. Imaging modalities help guide the embolization procedure but are not always reliable as seen in our case. Early angiographic and surgical intervention in refractory cases should be considered to prevent morbidity and mortality.
Disclosures:
Steven Kessler, BS1, Prekchha Jha, MBBS2, Mihaela Batke, MD2. P1994 - Bleeding Dieulafoy’s Lesion: Refractory to All Endoscopic Measures, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Oakland University William Beaumont School of Medicine, Rochester, MI; 2Corewell Health, Royal Oak, MI
Introduction: Dieulafoy’s lesion is a developmental vascular malformation often located in the stomach. One third can have extra gastric location, frequently the duodenum. These account for 1-2% of acute gastrointestinal (GI) bleeding. Prior to advancement in endoscopic techniques, mortality was as high as 80%. Endoscopic therapy success rate is reported to be 90%. We present a case of a bleeding duodenal Dieulafoy’s lesion refractory to endoscopic hemostasis.
Case Description/Methods: 75-year-old man with a prolonged hospital course after mitral valve replacement for infective endocarditis developed large melanotic stools at day 21 of admission. Esophagogastroduodenoscopy (EGD) showed a large bleeding Dieulafoy’s lesion in the second portion of the duodenum. Hemostasis was achieved with over the scope clip (OTSC). He continued to have low volume melena and required transfusion of 1-2 units of packed red blood cells (pRBC) every 1-2 days. EGD 2 weeks later showed active bleeding around edges of the OTSC, and was controlled by hemospray application. He continued to have melena and remained transfusion dependent. Interventional Radiology (IR) was consulted for empiric Gastro Duodenal Artery (GDA) embolization. Unfortunately, he had variant anatomy with duodenal vascularization from a Superior Mesenteric Artery (SMA) branch without active bleed. Empiric embolization was not performed due to concern of acute small bowel necrosis. Computed Tomography Angiography studies were negative. A third EGD revealed continued bleeding at the site of the OTSC. Attempts to attain hemostasis were made with 8 hemoclips and epinephrine injection but were unsuccessful. Temporary hemostasis was achieved with hemospray. At this point, all possible endoscopic means to achieve hemostasis were exhausted. IR was able to achieve definitive hemostasis after targeted embolization of the branch feeding the area of the Dieulafoy. Patient received a total of 38 units of pRBC in 50 days of hospitalization.
Discussion: Dieulafoy’s lesions can cause life threatening bleeding. Endoscopic hemostasis is the mainstay therapy but this is not always successful. Imaging modalities help guide the embolization procedure but are not always reliable as seen in our case. Early angiographic and surgical intervention in refractory cases should be considered to prevent morbidity and mortality.
Disclosures:
Steven Kessler indicated no relevant financial relationships.
Prekchha Jha indicated no relevant financial relationships.
Mihaela Batke indicated no relevant financial relationships.
Steven Kessler, BS1, Prekchha Jha, MBBS2, Mihaela Batke, MD2. P1994 - Bleeding Dieulafoy’s Lesion: Refractory to All Endoscopic Measures, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
