Monday Poster Session
Category: General Endoscopy
P1995 - Ileal Prolapse in Cecum Masquerading as a Cecal Polyp
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sandeep Verma, MD
Sinai Hospital
Baltimore, MD
Presenting Author(s)
Sandeep Verma, MD, Anisha Garg, MD, Sudhir K. Dutta, MD, MACG
Sinai Hospital, Baltimore, MD
Introduction: Ileal prolapse is an exceedingly rare presentation with only a few cases in the literature. Presentation can be completely asymptomatic and there are no notable predisposing factors for this condition.
Case Description/Methods: A 54 years F with PMH of mild ulcerative colitis (on stable mesalamine regimen) presented to endoscopy suite for routine colonoscopy. Physical exam findings including per rectal exam was essentially normal. Laboratory markers were unremarkable. Colonoscopy was performed which showed nonrevealing of any gross pathologies in the entire colon. A salmon colored localized area and a sausage like pseudo-polyp was found in the cecum. Plans were made to remove this lesion using endoscopic mucosal resection, on palpation with the forceps the lesion appeared to be soft. Air insufflation was performed to dilate the cecum for the resection. It was noted that the lesion started diminishing in size and it rapidly disappeared leaving a wide patent ileocecal opening. Multiple random biopsies were obtained from various parts of the colon for histology. The biopsy results of the polypoid lesion revealed that this was normal ileal mucosa with no significant pathological findings. Other biopsies from the different parts of the colon were also unremarkable without evidence of active IBD.
Discussion: Ileal prolapse is a rare presentation with only three reported cases in the world literature. Initial two cases with ileal prolapsed were based on barium studies in 1950s. These two cases ileal prolapse was as a filling defect consistent with a neoplastic lesion and the patients underwent ex-laparotomy which showed ileal prolapse into the cecum and no resection was done. In a more recent case, a similar characteristic large polypoidal lesion noted at ileocecal valve, however the lesion disappeared on withdrawal of colonoscope back into cecum.
Additionally, cases of ileal prolapse have been reported in patients with ileal pouch which was surgically created in patients with IBD. In a retrospective study, 11 patients were diagnosed with ileal prolapse out of 3176 ileal pouch, over a period of time. Out of these cases 7 had full thickness and 4 had mucosal prolapse. While the mucosal prolapse maybe treated with stool bulking, full thickness prolapse necessitates definitive surgery and is associated with risk of pouch loss.
Our case highlights the need for careful assessment of ileocolonic lesion to prevent misidentification as a pseudo polyp and unnecessary attempt to resect the lesion endoscopically.

Disclosures:
Sandeep Verma, MD, Anisha Garg, MD, Sudhir K. Dutta, MD, MACG. P1995 - Ileal Prolapse in Cecum Masquerading as a Cecal Polyp, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Sinai Hospital, Baltimore, MD
Introduction: Ileal prolapse is an exceedingly rare presentation with only a few cases in the literature. Presentation can be completely asymptomatic and there are no notable predisposing factors for this condition.
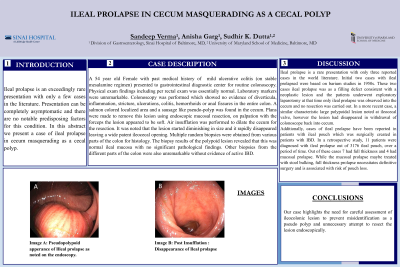
Case Description/Methods: A 54 years F with PMH of mild ulcerative colitis (on stable mesalamine regimen) presented to endoscopy suite for routine colonoscopy. Physical exam findings including per rectal exam was essentially normal. Laboratory markers were unremarkable. Colonoscopy was performed which showed nonrevealing of any gross pathologies in the entire colon. A salmon colored localized area and a sausage like pseudo-polyp was found in the cecum. Plans were made to remove this lesion using endoscopic mucosal resection, on palpation with the forceps the lesion appeared to be soft. Air insufflation was performed to dilate the cecum for the resection. It was noted that the lesion started diminishing in size and it rapidly disappeared leaving a wide patent ileocecal opening. Multiple random biopsies were obtained from various parts of the colon for histology. The biopsy results of the polypoid lesion revealed that this was normal ileal mucosa with no significant pathological findings. Other biopsies from the different parts of the colon were also unremarkable without evidence of active IBD.
Discussion: Ileal prolapse is a rare presentation with only three reported cases in the world literature. Initial two cases with ileal prolapsed were based on barium studies in 1950s. These two cases ileal prolapse was as a filling defect consistent with a neoplastic lesion and the patients underwent ex-laparotomy which showed ileal prolapse into the cecum and no resection was done. In a more recent case, a similar characteristic large polypoidal lesion noted at ileocecal valve, however the lesion disappeared on withdrawal of colonoscope back into cecum.
Additionally, cases of ileal prolapse have been reported in patients with ileal pouch which was surgically created in patients with IBD. In a retrospective study, 11 patients were diagnosed with ileal prolapse out of 3176 ileal pouch, over a period of time. Out of these cases 7 had full thickness and 4 had mucosal prolapse. While the mucosal prolapse maybe treated with stool bulking, full thickness prolapse necessitates definitive surgery and is associated with risk of pouch loss.
Our case highlights the need for careful assessment of ileocolonic lesion to prevent misidentification as a pseudo polyp and unnecessary attempt to resect the lesion endoscopically.

Figure: Ileal Prolapse Images
Disclosures:
Sandeep Verma indicated no relevant financial relationships.
Anisha Garg indicated no relevant financial relationships.
Sudhir K. Dutta indicated no relevant financial relationships.
Sandeep Verma, MD, Anisha Garg, MD, Sudhir K. Dutta, MD, MACG. P1995 - Ileal Prolapse in Cecum Masquerading as a Cecal Polyp, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
