Monday Poster Session
Category: General Endoscopy
P2005 - Traumatic Uvulitis: A Rare Complication of a Common Procedure
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- MA
Michael Adams, DO
Martin Army Community Hospital
Fort Moore, GA
Presenting Author(s)
Michael Adams, DO1, Carl Kay, MD2, Geoff Bader, MD3, Charles Miller, MD4
1Martin Army Community Hospital, Fort Moore, GA; 2Brooke Army Medical Center, Fort Sam Houston, TX; 3Brooke Army Medical Center, San Antonio, TX; 4San Antonio Uniformed Services Health Education Consortium, San Antonio, TX
Introduction: Esophagogastroduodenoscopy (EGD) is a common procedure with rare adverse events, usually related to anesthesia, infection, perforation, or bleeding. Uvulitis, or edema of the uvula, has many causes including infection, allergic reactions, caustic inhalation/injury, or trauma. Uvulitis, with or without necrosis, is a rare complication after an EGD. We describe a case of delayed traumatic uvulitis occurring after an EGD with moderate sedation and adjunctive topical lidocaine.
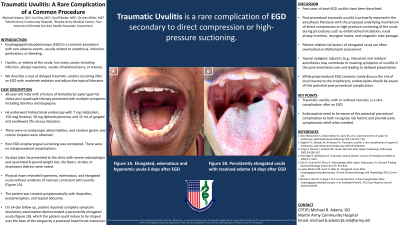
Case Description/Methods: A 30-year-old male with a history of Helicobacter pylori gastritis status post quadruple therapy presented with multiple symptoms including diarrhea and dyspepsia. He underwent bidirectional endoscopy with 7 mg midazolam, 150 mcg fentanyl, 50 mg diphenhydramine, and 15 mL of gargled and swallowed 2% viscous lidocaine. There were no endoscopic abnormalities, and random gastric and colonic biopsies were obtained. Post-EGD oropharyngeal suctioning was completed. There were no intraprocedural complications. Six days later, he presented to the clinic with severe odynophagia and associated 8-pound weight loss. No fevers, stridor, or respiratory distress were noted. Physical exam revealed hyperemic, edematous, and elongated uvula without evidence of necrosis consistent with uvulitis. The patient was treated symptomatically with ibuprofen, acetaminophen, and topical lidocaine. On 14-day follow up, patient reported complete symptom resolution; examination demonstrated a persistently elongated uvula which the patient could induce to be draped over the base of the tongue by a practiced head thrust maneuver.
Discussion: Post-procedural traumatic uvulitis is primarily reported in the anesthesia literature with the proposed underlying mechanism of direct compression or high-pressure suctioning of the uvula during procedures such as endotracheal intubation, nasal airway insertion, laryngeal masks, and orogastric tube passage. Few cases of post-EGD uvulitis have been described. Patient-related risk factors of elongated uvula are often overlooked on Mallampati assessment. Topical analgesic adjuncts (e.g., lidocaine) and residual anesthetics may contribute to masking symptoms of uvulitis in the post-anesthesia care unit leading to delayed presentation. While preprocedural EGD consents rarely discuss the risk of local trauma to the oropharynx, endoscopists should be aware of this potential post-procedural complication.

Disclosures:
Michael Adams, DO1, Carl Kay, MD2, Geoff Bader, MD3, Charles Miller, MD4. P2005 - Traumatic Uvulitis: A Rare Complication of a Common Procedure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Martin Army Community Hospital, Fort Moore, GA; 2Brooke Army Medical Center, Fort Sam Houston, TX; 3Brooke Army Medical Center, San Antonio, TX; 4San Antonio Uniformed Services Health Education Consortium, San Antonio, TX
Introduction: Esophagogastroduodenoscopy (EGD) is a common procedure with rare adverse events, usually related to anesthesia, infection, perforation, or bleeding. Uvulitis, or edema of the uvula, has many causes including infection, allergic reactions, caustic inhalation/injury, or trauma. Uvulitis, with or without necrosis, is a rare complication after an EGD. We describe a case of delayed traumatic uvulitis occurring after an EGD with moderate sedation and adjunctive topical lidocaine.
Case Description/Methods: A 30-year-old male with a history of Helicobacter pylori gastritis status post quadruple therapy presented with multiple symptoms including diarrhea and dyspepsia. He underwent bidirectional endoscopy with 7 mg midazolam, 150 mcg fentanyl, 50 mg diphenhydramine, and 15 mL of gargled and swallowed 2% viscous lidocaine. There were no endoscopic abnormalities, and random gastric and colonic biopsies were obtained. Post-EGD oropharyngeal suctioning was completed. There were no intraprocedural complications. Six days later, he presented to the clinic with severe odynophagia and associated 8-pound weight loss. No fevers, stridor, or respiratory distress were noted. Physical exam revealed hyperemic, edematous, and elongated uvula without evidence of necrosis consistent with uvulitis. The patient was treated symptomatically with ibuprofen, acetaminophen, and topical lidocaine. On 14-day follow up, patient reported complete symptom resolution; examination demonstrated a persistently elongated uvula which the patient could induce to be draped over the base of the tongue by a practiced head thrust maneuver.
Discussion: Post-procedural traumatic uvulitis is primarily reported in the anesthesia literature with the proposed underlying mechanism of direct compression or high-pressure suctioning of the uvula during procedures such as endotracheal intubation, nasal airway insertion, laryngeal masks, and orogastric tube passage. Few cases of post-EGD uvulitis have been described. Patient-related risk factors of elongated uvula are often overlooked on Mallampati assessment. Topical analgesic adjuncts (e.g., lidocaine) and residual anesthetics may contribute to masking symptoms of uvulitis in the post-anesthesia care unit leading to delayed presentation. While preprocedural EGD consents rarely discuss the risk of local trauma to the oropharynx, endoscopists should be aware of this potential post-procedural complication.

Figure: Figure 1A: Elongated, edematous and hyperemic uvula 6 days after EGD
Figure 1B: Persistently elongated uvula with resolved edematous uvula 14 days after EGD
Figure 1B: Persistently elongated uvula with resolved edematous uvula 14 days after EGD
Disclosures:
Michael Adams indicated no relevant financial relationships.
Carl Kay indicated no relevant financial relationships.
Geoff Bader indicated no relevant financial relationships.
Charles Miller indicated no relevant financial relationships.
Michael Adams, DO1, Carl Kay, MD2, Geoff Bader, MD3, Charles Miller, MD4. P2005 - Traumatic Uvulitis: A Rare Complication of a Common Procedure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
