Monday Poster Session
Category: GI Bleeding
P2034 - Management of Direct Acting Oral Anticoagulants in Hospitalized Patients With Upper Gastrointestinal Bleeding: A Real-World Observational Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Daniel Kats, MD
Yale-New Haven Hospital
New Haven, CT
Presenting Author(s)
Daniel Kats, MD1, Neil Zheng, BS2, Jack Huebner, MD1, Rumzah Paracha, MD1, Michelle Melo, MD3, Johannes DuPont, MSc2, Dennis Shung, MD, PhD2, Darrick K. Li, MD, PhD2
1Yale-New Haven Hospital, New Haven, CT; 2Yale School of Medicine, New Haven, CT; 3Yale-Waterbury Hospital, Waterbury, CT
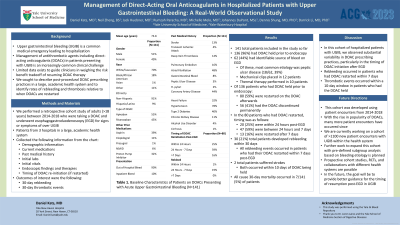
Introduction: Upper gastrointestinal bleeding (UGIB) remains a common medical emergency leading to hospitalization. Management of antithrombotic agents including direct acting oral anticoagulants (DOACs) in patients presenting with UGIB has become an increasingly common clinical challenge. Limited data exists to guide clinicians in weighing the risk benefit tradeoff of resuming DOAC therapy. We sought to describe post-procedural DOAC prescribing practices in a large, academic health system and to identify rates of rebleeding and thrombosis relative to when DOACs are restarted.
Methods: We performed a retrospective cohort study of adults ( >18 years) between 2014-2018 who were taking a DOAC and underwent esophagogastroduodenoscopy (EGD) for signs or symptoms of overt UGIB within 3 hospitals in a large academic hospital system. Demographic information, current medications, past medical history, initial labs, vitals, endoscopic findings, and timing of DOAC re-initiation were extracted from the chart. Outcomes of interest were 30-day rebleeding and thrombotic events.
Results: Among 141 patients included in the study, 136 (96%) had DOAC held prior to endoscopy. 62 (44%) had an identifiable source on EGD, and of these, the most common etiology was peptic ulcer disease (18/62, 29%). Mechanical clips were placed in 12 patients while thermal therapy was performed in 10 patients. Of 136 patients who had DOAC held prior to endoscopy, 80 (59%) were restarted while 56 (41%) had their DOAC discontinued permanently. Overall, 30 patients developed rebleeding (21%). Regarding timing of DOAC re-initiation, 20/80 (25%) were restarted within 24 hours post-EGD; 47/80 (59%) between 24 hours and 7 days; 13/80 (14%) were restarted after 7 days. All rebleeding events occurred in patients who had their DOAC restarted within 7 days. 2 patients suffered strokes, both occurring within 10 days of DOAC being held. All-cause 30-day mortality occurred in 7/141 (5%) patients.
Discussion: In this cohort of hospitalized patients with UGIB, we observed substantial variability in DOAC prescribing practices, particularly in the timing of DOAC initiation after EGD. Rebleeding occurred in patients who had the DOAC restarted within 7 days, though thrombotic events occurred within a 10-day window in patients who had the DOAC held. Further work to expand this cohort with pre-defined subgroup analysis based on bleeding etiology is planned.
Disclosures:
Daniel Kats, MD1, Neil Zheng, BS2, Jack Huebner, MD1, Rumzah Paracha, MD1, Michelle Melo, MD3, Johannes DuPont, MSc2, Dennis Shung, MD, PhD2, Darrick K. Li, MD, PhD2. P2034 - Management of Direct Acting Oral Anticoagulants in Hospitalized Patients With Upper Gastrointestinal Bleeding: A Real-World Observational Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Yale-New Haven Hospital, New Haven, CT; 2Yale School of Medicine, New Haven, CT; 3Yale-Waterbury Hospital, Waterbury, CT
Introduction: Upper gastrointestinal bleeding (UGIB) remains a common medical emergency leading to hospitalization. Management of antithrombotic agents including direct acting oral anticoagulants (DOACs) in patients presenting with UGIB has become an increasingly common clinical challenge. Limited data exists to guide clinicians in weighing the risk benefit tradeoff of resuming DOAC therapy. We sought to describe post-procedural DOAC prescribing practices in a large, academic health system and to identify rates of rebleeding and thrombosis relative to when DOACs are restarted.
Methods: We performed a retrospective cohort study of adults ( >18 years) between 2014-2018 who were taking a DOAC and underwent esophagogastroduodenoscopy (EGD) for signs or symptoms of overt UGIB within 3 hospitals in a large academic hospital system. Demographic information, current medications, past medical history, initial labs, vitals, endoscopic findings, and timing of DOAC re-initiation were extracted from the chart. Outcomes of interest were 30-day rebleeding and thrombotic events.
Results: Among 141 patients included in the study, 136 (96%) had DOAC held prior to endoscopy. 62 (44%) had an identifiable source on EGD, and of these, the most common etiology was peptic ulcer disease (18/62, 29%). Mechanical clips were placed in 12 patients while thermal therapy was performed in 10 patients. Of 136 patients who had DOAC held prior to endoscopy, 80 (59%) were restarted while 56 (41%) had their DOAC discontinued permanently. Overall, 30 patients developed rebleeding (21%). Regarding timing of DOAC re-initiation, 20/80 (25%) were restarted within 24 hours post-EGD; 47/80 (59%) between 24 hours and 7 days; 13/80 (14%) were restarted after 7 days. All rebleeding events occurred in patients who had their DOAC restarted within 7 days. 2 patients suffered strokes, both occurring within 10 days of DOAC being held. All-cause 30-day mortality occurred in 7/141 (5%) patients.
Discussion: In this cohort of hospitalized patients with UGIB, we observed substantial variability in DOAC prescribing practices, particularly in the timing of DOAC initiation after EGD. Rebleeding occurred in patients who had the DOAC restarted within 7 days, though thrombotic events occurred within a 10-day window in patients who had the DOAC held. Further work to expand this cohort with pre-defined subgroup analysis based on bleeding etiology is planned.
Disclosures:
Daniel Kats indicated no relevant financial relationships.
Neil Zheng indicated no relevant financial relationships.
Jack Huebner indicated no relevant financial relationships.
Rumzah Paracha indicated no relevant financial relationships.
Michelle Melo indicated no relevant financial relationships.
Johannes DuPont indicated no relevant financial relationships.
Dennis Shung indicated no relevant financial relationships.
Darrick Li indicated no relevant financial relationships.
Daniel Kats, MD1, Neil Zheng, BS2, Jack Huebner, MD1, Rumzah Paracha, MD1, Michelle Melo, MD3, Johannes DuPont, MSc2, Dennis Shung, MD, PhD2, Darrick K. Li, MD, PhD2. P2034 - Management of Direct Acting Oral Anticoagulants in Hospitalized Patients With Upper Gastrointestinal Bleeding: A Real-World Observational Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

