Monday Poster Session
Category: GI Bleeding
P2040 - Comparison of Alternative Upper GI Bleeding Risk Assessments With Time to Scope and Mortality
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Monica Arora, DO
St. Elizabeth Youngstown Hospital/NEOMED
Presenting Author(s)
Monica Arora, DO, Mohammad Qazziha, MBBS, Maria Veronica Mirano-De Guzman, MD, MBA, Feruza Abraamyan, MD, Sean Mohtashami, BS, Robert Douglass, BS, David Gemmel, PhD, Timothy Barreiro, DO, MPH
St. Elizabeth Youngstown Hospital/NEOMED, Youngstown, OH
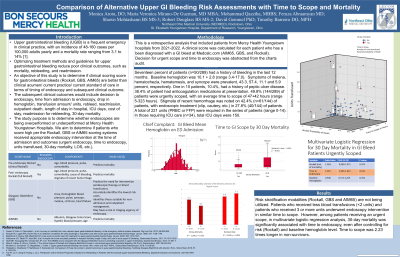
Introduction: Upper gastrointestinal bleeding (UGIB) has an incidence of 48-160 cases per 100,000 adults yearly and a mortality of 3.1-14%. Optimizing treatment methods and guidelines for UGIB reduce poor clinical outcomes (mortality,rebleeding,and readmission). We aim to determine if clinical scoring score for UGIB (Rockall,GBS,AIM65) are better than clinical acumen in terms of timing of endoscopy and subsequent clinical outcome. The clinical outcomes would include decision to endoscopy, time from admission to endoscopy, drop in hemoglobin, transfusion amount, rebleed, readmission, outpatient death, length of stay in hospital, ICU days, 30-day mortality. We aim to determine if patients who score high per the Rockall, GBS or AIM65 received appropriate endoscopy intervention at the time of admission and outcomes.
Methods: This was a retrospective analysis including patients (n=182) from a community hospital from 2021-2022. A clinical score was calculated for each patient who had been diagnosed with UGIB for risk stratification to determine need for urgent endoscopy, bleeding readmission, and mortality. Time to scope was also abstracted.
Results: 20.3% of patients had a history of bleeding in the last 12 months.Baseline hemoglobin was 10.8+/- 3.0 (range 3.4-17.0).Symptoms of melena, hematochezia, hematemesis, and syncope were prevalent, 42.3, 53.3, 9.9, and 8.8 percent, respectfully.11.5% of patients had a history of peptic ulcer disease. 39.0% of patients were on anticoagulation medications. 47.8% of patients (87/182) were urgently scoped, with an average time to scope of 56 hours (range 5-323 hours). Stigmata of recent hemorrhage was noted on 43/87 patients, with endoscopic treatment (clip, cautery, etc.) noted in 30/87 of these patients. A total of 170 units (PRBC or FFP) were required in this series of patients (range 0-14). In those requiring ICU care (n=25), total ICU days was 52.
Discussion: Risk stratification modalities (Rockall,GBS and AIM65) are not being utilized. Patients who received less blood transfusions underwent endoscopic intervention in 24-48 hours. Pt’s who received 3 or more units underwent endoscopy intervention in over 48 hours. In multivariate analysis, units transfused was significantly associated with time to endoscopy, even after controlling for risk and baseline hemoglobin level. In logistic regression, 30-day mortality was also associated with time to scope, controlling for Rockall risk stratification and baseline hemoglobin. Time to scope was 3x longer in non-survivors.
Disclosures:
Monica Arora, DO, Mohammad Qazziha, MBBS, Maria Veronica Mirano-De Guzman, MD, MBA, Feruza Abraamyan, MD, Sean Mohtashami, BS, Robert Douglass, BS, David Gemmel, PhD, Timothy Barreiro, DO, MPH. P2040 - Comparison of Alternative Upper GI Bleeding Risk Assessments With Time to Scope and Mortality, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
St. Elizabeth Youngstown Hospital/NEOMED, Youngstown, OH
Introduction: Upper gastrointestinal bleeding (UGIB) has an incidence of 48-160 cases per 100,000 adults yearly and a mortality of 3.1-14%. Optimizing treatment methods and guidelines for UGIB reduce poor clinical outcomes (mortality,rebleeding,and readmission). We aim to determine if clinical scoring score for UGIB (Rockall,GBS,AIM65) are better than clinical acumen in terms of timing of endoscopy and subsequent clinical outcome. The clinical outcomes would include decision to endoscopy, time from admission to endoscopy, drop in hemoglobin, transfusion amount, rebleed, readmission, outpatient death, length of stay in hospital, ICU days, 30-day mortality. We aim to determine if patients who score high per the Rockall, GBS or AIM65 received appropriate endoscopy intervention at the time of admission and outcomes.
Methods: This was a retrospective analysis including patients (n=182) from a community hospital from 2021-2022. A clinical score was calculated for each patient who had been diagnosed with UGIB for risk stratification to determine need for urgent endoscopy, bleeding readmission, and mortality. Time to scope was also abstracted.
Results: 20.3% of patients had a history of bleeding in the last 12 months.Baseline hemoglobin was 10.8+/- 3.0 (range 3.4-17.0).Symptoms of melena, hematochezia, hematemesis, and syncope were prevalent, 42.3, 53.3, 9.9, and 8.8 percent, respectfully.11.5% of patients had a history of peptic ulcer disease. 39.0% of patients were on anticoagulation medications. 47.8% of patients (87/182) were urgently scoped, with an average time to scope of 56 hours (range 5-323 hours). Stigmata of recent hemorrhage was noted on 43/87 patients, with endoscopic treatment (clip, cautery, etc.) noted in 30/87 of these patients. A total of 170 units (PRBC or FFP) were required in this series of patients (range 0-14). In those requiring ICU care (n=25), total ICU days was 52.
Discussion: Risk stratification modalities (Rockall,GBS and AIM65) are not being utilized. Patients who received less blood transfusions underwent endoscopic intervention in 24-48 hours. Pt’s who received 3 or more units underwent endoscopy intervention in over 48 hours. In multivariate analysis, units transfused was significantly associated with time to endoscopy, even after controlling for risk and baseline hemoglobin level. In logistic regression, 30-day mortality was also associated with time to scope, controlling for Rockall risk stratification and baseline hemoglobin. Time to scope was 3x longer in non-survivors.
Disclosures:
Monica Arora indicated no relevant financial relationships.
Mohammad Qazziha indicated no relevant financial relationships.
Maria Veronica Mirano-De Guzman indicated no relevant financial relationships.
Feruza Abraamyan indicated no relevant financial relationships.
Sean Mohtashami indicated no relevant financial relationships.
Robert Douglass indicated no relevant financial relationships.
David Gemmel indicated no relevant financial relationships.
Timothy Barreiro indicated no relevant financial relationships.
Monica Arora, DO, Mohammad Qazziha, MBBS, Maria Veronica Mirano-De Guzman, MD, MBA, Feruza Abraamyan, MD, Sean Mohtashami, BS, Robert Douglass, BS, David Gemmel, PhD, Timothy Barreiro, DO, MPH. P2040 - Comparison of Alternative Upper GI Bleeding Risk Assessments With Time to Scope and Mortality, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
