Monday Poster Session
Category: GI Bleeding
P2049 - A Challenging Case of Zollinger-Ellison Syndrome Presenting With Refractory Bleeding: Is There a Role for Upper Endoscopy Prior to Kidney Transplant?
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Michael Gianarakis, MD
University of Illinois at Chicago
Chicago, IL
Presenting Author(s)
Michael Gianarakis, MD, Elie Ghoulam, MD, Enrico Benedetti, MD, Robert Carroll, MD
University of Illinois at Chicago, Chicago, IL
Introduction: Zollinger-Ellison Syndrome (ZES) is a gastrin-secreting neuroendocrine tumor commonly located in the duodenum or pancreas that stimulates excess gastric acid production. It typically presents with peptic ulcer disease (PUD) symptoms such as abdominal pain and diarrhea, but advanced disease may present with signs of gastrointestinal bleeding (GIB). We present a case of ZES with refractory GIB following living donor kidney transplant (LDKT).
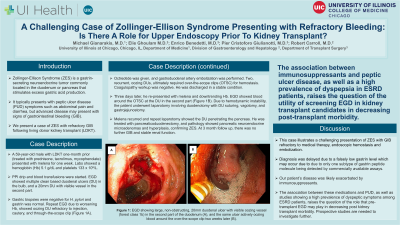
Case Description/Methods: A 59-year-old male with LDKT one-month prior (treated with prednisone, tacrolimus, mycophenolate) presented with melena for one week. Labs showed a hemoglobin (Hb) 5.1 g/dL and platelets 133 x 109/L. PPI drip and blood transfusions were started. EGD showed multiple clean based duodenal ulcers (DU) in the bulb, and a 20mm DU with visible vessel in the second part. Gastric biopsies were negative for H. pylori and gastrin was normal. Repeat EGD due to worsening Hb, showed oozing DU refractory to injection, cautery, and through-the-scope clip (Figure 1A). Octreotide was given, and gastroduodenal artery embolization was performed. Two, recurrent, oozing DUs, ultimately required over-the-scope clips (OTSC) for hemostasis. Coagulopathy workup was negative. He was discharged in a stable condition.
Three days later, he re-presented with melena and downtrending Hb. EGD showed blood around the OTSC at the DU in the second part (Figure 1B). Due to hemodynamic instability, the patient underwent laparotomy involving duodenotomy with DU suturing, vagotomy, and gastrojejunostomy. Melena recurred and repeat laparotomy showed the DU penetrating the pancreas. He was treated with pancreaticoduodenectomy, and pathology showed pancreatic neuroendocrine microadenomas and hyperplasia, confirming ZES. At 3 month follow up, there was no further GIB and stable renal function.
Discussion: This case illustrates a challenging presentation of ZES with GIB refractory to medical therapy, endoscopic hemostasis, and embolization. Diagnosis was delayed due to a falsely low gastrin level, which may occur due to only one subtype of gastrin peptide molecule being detected by commercially available assays. Our patient's disease was likely exacerbated by immunosuppressants. The association between these medications and PUD, as well as studies showing a high prevalence of dyspeptic symptoms among ESRD patients, raises the question of the role that pre-transplant EGD may play in decreasing post kidney transplant morbidity. Prospective studies are needed to investigate further.

Disclosures:
Michael Gianarakis, MD, Elie Ghoulam, MD, Enrico Benedetti, MD, Robert Carroll, MD. P2049 - A Challenging Case of Zollinger-Ellison Syndrome Presenting With Refractory Bleeding: Is There a Role for Upper Endoscopy Prior to Kidney Transplant?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Illinois at Chicago, Chicago, IL
Introduction: Zollinger-Ellison Syndrome (ZES) is a gastrin-secreting neuroendocrine tumor commonly located in the duodenum or pancreas that stimulates excess gastric acid production. It typically presents with peptic ulcer disease (PUD) symptoms such as abdominal pain and diarrhea, but advanced disease may present with signs of gastrointestinal bleeding (GIB). We present a case of ZES with refractory GIB following living donor kidney transplant (LDKT).
Case Description/Methods: A 59-year-old male with LDKT one-month prior (treated with prednisone, tacrolimus, mycophenolate) presented with melena for one week. Labs showed a hemoglobin (Hb) 5.1 g/dL and platelets 133 x 109/L. PPI drip and blood transfusions were started. EGD showed multiple clean based duodenal ulcers (DU) in the bulb, and a 20mm DU with visible vessel in the second part. Gastric biopsies were negative for H. pylori and gastrin was normal. Repeat EGD due to worsening Hb, showed oozing DU refractory to injection, cautery, and through-the-scope clip (Figure 1A). Octreotide was given, and gastroduodenal artery embolization was performed. Two, recurrent, oozing DUs, ultimately required over-the-scope clips (OTSC) for hemostasis. Coagulopathy workup was negative. He was discharged in a stable condition.
Three days later, he re-presented with melena and downtrending Hb. EGD showed blood around the OTSC at the DU in the second part (Figure 1B). Due to hemodynamic instability, the patient underwent laparotomy involving duodenotomy with DU suturing, vagotomy, and gastrojejunostomy. Melena recurred and repeat laparotomy showed the DU penetrating the pancreas. He was treated with pancreaticoduodenectomy, and pathology showed pancreatic neuroendocrine microadenomas and hyperplasia, confirming ZES. At 3 month follow up, there was no further GIB and stable renal function.
Discussion: This case illustrates a challenging presentation of ZES with GIB refractory to medical therapy, endoscopic hemostasis, and embolization. Diagnosis was delayed due to a falsely low gastrin level, which may occur due to only one subtype of gastrin peptide molecule being detected by commercially available assays. Our patient's disease was likely exacerbated by immunosuppressants. The association between these medications and PUD, as well as studies showing a high prevalence of dyspeptic symptoms among ESRD patients, raises the question of the role that pre-transplant EGD may play in decreasing post kidney transplant morbidity. Prospective studies are needed to investigate further.

Figure: EGD showing large, non-obstructing, 20mm duodenal ulcer with visible oozing vessel (forest class 1b) in the second part of the duodenum (A), and the same ulcer actively oozing blood around the over-the-scope clip two weeks later (B).
Disclosures:
Michael Gianarakis indicated no relevant financial relationships.
Elie Ghoulam indicated no relevant financial relationships.
Enrico Benedetti indicated no relevant financial relationships.
Robert Carroll: Takedz – Speakers Bureau.
Michael Gianarakis, MD, Elie Ghoulam, MD, Enrico Benedetti, MD, Robert Carroll, MD. P2049 - A Challenging Case of Zollinger-Ellison Syndrome Presenting With Refractory Bleeding: Is There a Role for Upper Endoscopy Prior to Kidney Transplant?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
