Monday Poster Session
Category: GI Bleeding
P2086 - Double-Balloon Enteroscopy in the Management of Overt Gastrointestinal Bleeding From a Rare Ileal Arteriovenous Malformation
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Clive J. Miranda, DO, MS
University at Buffalo
Buffalo, NY
Presenting Author(s)
Clive J. Miranda, DO, MS, Farhan Azad, DO, Alexander M. Carlson, DO, Muddasir Ayaz, MD
University at Buffalo, Buffalo, NY
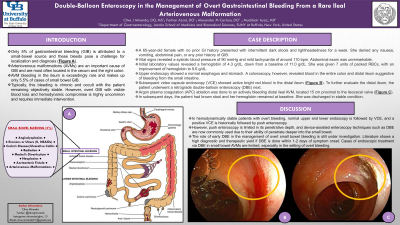
Introduction: Only 5% of gastrointestinal bleeding (GIB) is attributed to a small-bowel source and these bleeds pose a challenge for localization and diagnosis. Arteriovenous malformations (AVMs) are an important cause of GIB and are most often located in the cecum and the right colon. AVM bleeding in the ileum is exceedingly rare and makes up only 5.5% of cases of small bowel GIB. Typically, this bleeding is chronic and occult with the patient remaining objectively stable. However, overt GIB with visible blood loss and hemodynamic compromise is highly uncommon and requires immediate intervention.
Case Description/Methods: A 65-year-old female with no prior GI history presented with intermittent dark stools and lightheadedness for a week. She denied any nausea, vomiting, abdominal pain, or any prior history of GIB. Vital signs revealed a systolic blood pressure of 90 mmHg and mild tachycardia of around 110 bpm. Abdominal exam was unremarkable. Initial laboratory values revealed a hemoglobin of 4.3 g/dL, down from a baseline of 11.0 g/dL. She was given 7 units of packed RBCs, with an improvement of hemoglobin to 9.6 g/dL. An upper endoscopy was performed showing a normal esophagus and stomach. A colonoscopy, however, revealed blood in the entire colon and distal ileum suggestive of bleeding from the small intestine. A subsequent video capsule endoscopy (VCE) showed active bright red blood in the distal ileum (Figure 1). To further evaluate the distal ileum, the patient underwent a retrograde double-balloon enteroscopy (DBE) next. Argon plasma coagulation (APC) ablation was done to an actively bleeding distal ileal AVM, located 15 cm proximal to the ileocecal valve (Figure 2). In subsequent days, the patient had brown stool and her hemoglobin remained at baseline. She was discharged in stable condition.
Discussion: In hemodynamically stable patients with overt bleeding, normal upper and lower endoscopy is followed by VCE, and a positive VCE is historically followed by push enteroscopy. However, push enteroscopy is limited in its penetrative depth, and device-assisted enteroscopy techniques such as DBE are now commonly used due to their ability of penetrate deeper into the small bowel. The role of early DBE in the management of overt small bowel bleeding is still under investigation. Literature shows a high diagnostic and therapeutic yield if DBE is done within 1-2 days of symptom onset. Cases of endoscopic treatment via DBE in small bowel AVMs are limited, especially in the setting of overt bleeding.

Disclosures:
Clive J. Miranda, DO, MS, Farhan Azad, DO, Alexander M. Carlson, DO, Muddasir Ayaz, MD. P2086 - Double-Balloon Enteroscopy in the Management of Overt Gastrointestinal Bleeding From a Rare Ileal Arteriovenous Malformation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University at Buffalo, Buffalo, NY
Introduction: Only 5% of gastrointestinal bleeding (GIB) is attributed to a small-bowel source and these bleeds pose a challenge for localization and diagnosis. Arteriovenous malformations (AVMs) are an important cause of GIB and are most often located in the cecum and the right colon. AVM bleeding in the ileum is exceedingly rare and makes up only 5.5% of cases of small bowel GIB. Typically, this bleeding is chronic and occult with the patient remaining objectively stable. However, overt GIB with visible blood loss and hemodynamic compromise is highly uncommon and requires immediate intervention.
Case Description/Methods: A 65-year-old female with no prior GI history presented with intermittent dark stools and lightheadedness for a week. She denied any nausea, vomiting, abdominal pain, or any prior history of GIB. Vital signs revealed a systolic blood pressure of 90 mmHg and mild tachycardia of around 110 bpm. Abdominal exam was unremarkable. Initial laboratory values revealed a hemoglobin of 4.3 g/dL, down from a baseline of 11.0 g/dL. She was given 7 units of packed RBCs, with an improvement of hemoglobin to 9.6 g/dL. An upper endoscopy was performed showing a normal esophagus and stomach. A colonoscopy, however, revealed blood in the entire colon and distal ileum suggestive of bleeding from the small intestine. A subsequent video capsule endoscopy (VCE) showed active bright red blood in the distal ileum (Figure 1). To further evaluate the distal ileum, the patient underwent a retrograde double-balloon enteroscopy (DBE) next. Argon plasma coagulation (APC) ablation was done to an actively bleeding distal ileal AVM, located 15 cm proximal to the ileocecal valve (Figure 2). In subsequent days, the patient had brown stool and her hemoglobin remained at baseline. She was discharged in stable condition.
Discussion: In hemodynamically stable patients with overt bleeding, normal upper and lower endoscopy is followed by VCE, and a positive VCE is historically followed by push enteroscopy. However, push enteroscopy is limited in its penetrative depth, and device-assisted enteroscopy techniques such as DBE are now commonly used due to their ability of penetrate deeper into the small bowel. The role of early DBE in the management of overt small bowel bleeding is still under investigation. Literature shows a high diagnostic and therapeutic yield if DBE is done within 1-2 days of symptom onset. Cases of endoscopic treatment via DBE in small bowel AVMs are limited, especially in the setting of overt bleeding.

Figure: Figure 1: Video capsule endoscopy showing active bright red blood in the distal ileum.
Figure 2: Endoscopic visualization status-post argon plasma coagulation to an actively bleeding distal ileal AVM
Figure 2: Endoscopic visualization status-post argon plasma coagulation to an actively bleeding distal ileal AVM
Disclosures:
Clive Miranda indicated no relevant financial relationships.
Farhan Azad indicated no relevant financial relationships.
Alexander Carlson indicated no relevant financial relationships.
Muddasir Ayaz indicated no relevant financial relationships.
Clive J. Miranda, DO, MS, Farhan Azad, DO, Alexander M. Carlson, DO, Muddasir Ayaz, MD. P2086 - Double-Balloon Enteroscopy in the Management of Overt Gastrointestinal Bleeding From a Rare Ileal Arteriovenous Malformation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
