Monday Poster Session
Category: IBD
P2119 - Integrating Routine Remote Patient Reported Outcomes Into Inflammatory Bowel Disease Care: A Rapid Qualitative Analysis of CAPTURE-IBD Intervention Participants
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Daniel Aintabi, MD, MSc
Trinity Health Ann Arbor Hospital
Ann Arbor, MI
Presenting Author(s)
Daniel Aintabi, MD, MSc1, Gillian Greenberg, MD2, Daniel Wray, MSc3, Melissa DeJonckheere, PhD4, Peter Higgins, MD, PhD, MSc5, Jeffrey Berinstein, MD, MSc5, Shirley Cohen-Mekelburg, MD, MS6
1Trinity Health Ann Arbor Hospital, Ann Arbor, MI; 2Children's Hospital of Michigan, Berkley, MI; 3Twine Clinical Consulting, Park City, UT; 4University of Michigan Medical School, Ann Arbor, MI; 5University of Michigan Hospital, Ann Arbor, MI; 6University of Michigan, Ann Arbor, MI
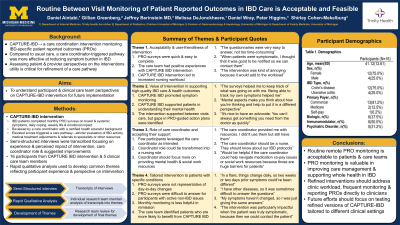
Introduction: In a recent randomized controlled trial, the routine remote collection of patient-reported outcomes (PRO) and care coordinator-triggered care pathways (the CAPTURE-IBD intervention) was more efficacious in reducing patients’ symptom burden as compared to usual care. Using a process evaluation, we evaluated patient and clinician perspectives and experiences with CAPTURE-IBD, to prepare for real world deployment of a refined intervention.
Methods: We conducted post-intervention interviews with a sample of trial participants and their clinicians (nurses, gastroenterologists). Interview questions elicited information from four key domains regarding experience with the intervention, its perceived impact, the care coordinator role, and suggested improvements. Using rapid qualitative analysis methods, we created a summary of each interview using a structured template, and transferred interview summaries into a matrix by domain, allowing us to compare individual experiences and perceptions.
Results: We conducted interviews with 16 patients and 4 clinicians. Interview summary details are reported in Table 1. Patients and clinicians found value in the remote monitoring of symptoms and facilitation in patient-care team communication. Several patients did not perceive a benefit from the intervention in the context of inactive IBD or confidence navigating healthcare. Participants found monthly remote PRO monitoring to be feasible and acceptable, though several participants felt more frequent monitoring would better represent their lived experiences. Few participants utilized care coordinator resources. Ultimately, participants suggested the CAPTURE-IBD intervention could be refined with more transparent PRO-guided decisions, and was best suited to patients with active symptoms, without comorbid illnesses, who lack sufficient self-care skills. Clinicians experienced increased workload, and there were concerns that a nurse would be better suited to the care coordinator role to minimize redundancy in PRO-guided decision making. They also suggested added value to clear PRO-guided actions and targeting psychosocial barriers.
Discussion: Patients and clinicians find value in integrating PROs into routine remote IBD care. A refined intervention should address clinic workload, include more frequent monitoring, and consider reporting PROs directly to clinicians. Future work should consider individually tailoring the intervention to patients’ IBD activity and comorbid illnesses.
Disclosures:
Daniel Aintabi, MD, MSc1, Gillian Greenberg, MD2, Daniel Wray, MSc3, Melissa DeJonckheere, PhD4, Peter Higgins, MD, PhD, MSc5, Jeffrey Berinstein, MD, MSc5, Shirley Cohen-Mekelburg, MD, MS6. P2119 - Integrating Routine Remote Patient Reported Outcomes Into Inflammatory Bowel Disease Care: A Rapid Qualitative Analysis of CAPTURE-IBD Intervention Participants, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Trinity Health Ann Arbor Hospital, Ann Arbor, MI; 2Children's Hospital of Michigan, Berkley, MI; 3Twine Clinical Consulting, Park City, UT; 4University of Michigan Medical School, Ann Arbor, MI; 5University of Michigan Hospital, Ann Arbor, MI; 6University of Michigan, Ann Arbor, MI
Introduction: In a recent randomized controlled trial, the routine remote collection of patient-reported outcomes (PRO) and care coordinator-triggered care pathways (the CAPTURE-IBD intervention) was more efficacious in reducing patients’ symptom burden as compared to usual care. Using a process evaluation, we evaluated patient and clinician perspectives and experiences with CAPTURE-IBD, to prepare for real world deployment of a refined intervention.
Methods: We conducted post-intervention interviews with a sample of trial participants and their clinicians (nurses, gastroenterologists). Interview questions elicited information from four key domains regarding experience with the intervention, its perceived impact, the care coordinator role, and suggested improvements. Using rapid qualitative analysis methods, we created a summary of each interview using a structured template, and transferred interview summaries into a matrix by domain, allowing us to compare individual experiences and perceptions.
Results: We conducted interviews with 16 patients and 4 clinicians. Interview summary details are reported in Table 1. Patients and clinicians found value in the remote monitoring of symptoms and facilitation in patient-care team communication. Several patients did not perceive a benefit from the intervention in the context of inactive IBD or confidence navigating healthcare. Participants found monthly remote PRO monitoring to be feasible and acceptable, though several participants felt more frequent monitoring would better represent their lived experiences. Few participants utilized care coordinator resources. Ultimately, participants suggested the CAPTURE-IBD intervention could be refined with more transparent PRO-guided decisions, and was best suited to patients with active symptoms, without comorbid illnesses, who lack sufficient self-care skills. Clinicians experienced increased workload, and there were concerns that a nurse would be better suited to the care coordinator role to minimize redundancy in PRO-guided decision making. They also suggested added value to clear PRO-guided actions and targeting psychosocial barriers.
Discussion: Patients and clinicians find value in integrating PROs into routine remote IBD care. A refined intervention should address clinic workload, include more frequent monitoring, and consider reporting PROs directly to clinicians. Future work should consider individually tailoring the intervention to patients’ IBD activity and comorbid illnesses.
Disclosures:
Daniel Aintabi indicated no relevant financial relationships.
Gillian Greenberg indicated no relevant financial relationships.
Daniel Wray: Twine Clinical Consulting – Consultant.
Melissa DeJonckheere indicated no relevant financial relationships.
Peter Higgins: AbbVie – Consultant. Amgen – Consultant. Buhlmann Laboratories – Consultant. Celltrion – Consultant. Curacle – Consultant. Eli Lilly – Consultant. Genentech – Consultant.
Jeffrey Berinstein: Bristol Myers Squibb – Consultant. Buhlman Diagnostics – Consultant. Oshi Health – Consultant.
Shirley Cohen-Mekelburg indicated no relevant financial relationships.
Daniel Aintabi, MD, MSc1, Gillian Greenberg, MD2, Daniel Wray, MSc3, Melissa DeJonckheere, PhD4, Peter Higgins, MD, PhD, MSc5, Jeffrey Berinstein, MD, MSc5, Shirley Cohen-Mekelburg, MD, MS6. P2119 - Integrating Routine Remote Patient Reported Outcomes Into Inflammatory Bowel Disease Care: A Rapid Qualitative Analysis of CAPTURE-IBD Intervention Participants, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
