Monday Poster Session
Category: IBD
P2138 - Upadacitinib in Ulcerative Colitis: Early Experience From a Large Regional Health System
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- SD
Stavros Doumas, MD, MSc
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Stavros Doumas, MD, MSc1, Sophia Dahmani, BSc2, Harjit Singh, MD1, Peter Chi, BSN1, Mark Mattar, MD1
1MedStar Georgetown University Hospital, Washington, DC; 2Georgetown University Medical School, Washington, DC
Introduction: The discovery of biologic agents two decades ago has transformed ulcerative colitis (UC) therapeutics, as biologics are now considered the mainstay of treatment. Despite these treatment advances, a significant number of patients develop relapses and experience refractory disease or major side effects while on biologics. The recent approval of upadacitinib, an oral small molecule selective JAK1 inhibitor, has expanded our therapeutic armamentarium, but there is a paucity of reports describing real-world outcomes in UC. In this setting, we report our early experience in a large regional health system.
Methods: We identified UC patients that were prescribed Upadacitinib between June 1st , 2022, to February 6th, 2023, within the MedStar Health System. Inclusion criteria included: age >18 years, histological diagnosis of UC, and upadacitinib prescribed and filled at any MedStar Gastroenterology clinic site.
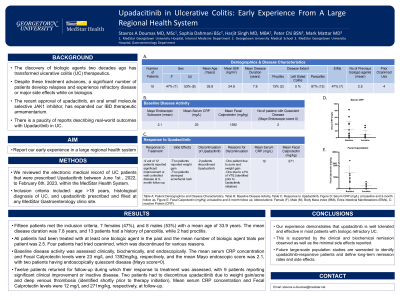
Results: Fifteen patients met the inclusion criteria, 7 females (47%), and 8 males (53%) with a mean age of 33.9 years. The mean disease duration was 7.8 years, and 13 patients had a history of pancolitis, while 2 had proctitis. All patients had been treated with at least one biologic agent in the past and the mean number of biologic agent trials per patient was 2.5. Four patients had tried ozanimod, which was discontinued for various reasons. We assessed baseline disease activity clinically, biochemically, and endoscopically. The mean serum CRP concentration and Fecal Calprotectin levels were 23 mg/L and 1392mg/kg, respectively, and the mean Mayo endoscopic score was 2.1, with two patients having endoscopically quiescent disease (Mayo score=0). Twelve patients returned for follow-up during which their response to treatment was assessed, with 9 patients reporting significant clinical improvement or inactive disease. Two patients had to discontinue upadacitinib due to weight gain/acne and deep venous thrombosis (identified shortly prior to therapy initiation). Mean serum CRP concentration and Fecal Calprotectin levels were 12 mg/L and 271mg/kg, respectively, at follow-up.
Discussion: Our experience demonstrates that upadacitinib is well tolerated and effective in most patients with biologic refractory UC. This is supported by the clinical and biochemical remission observed as well as the minimal side effects reported. Future large-scale population studies are warranted to identify upadacitinib-responsive patients and define long-term remission rates and side effects.

Disclosures:
Stavros Doumas, MD, MSc1, Sophia Dahmani, BSc2, Harjit Singh, MD1, Peter Chi, BSN1, Mark Mattar, MD1. P2138 - Upadacitinib in Ulcerative Colitis: Early Experience From a Large Regional Health System, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1MedStar Georgetown University Hospital, Washington, DC; 2Georgetown University Medical School, Washington, DC
Introduction: The discovery of biologic agents two decades ago has transformed ulcerative colitis (UC) therapeutics, as biologics are now considered the mainstay of treatment. Despite these treatment advances, a significant number of patients develop relapses and experience refractory disease or major side effects while on biologics. The recent approval of upadacitinib, an oral small molecule selective JAK1 inhibitor, has expanded our therapeutic armamentarium, but there is a paucity of reports describing real-world outcomes in UC. In this setting, we report our early experience in a large regional health system.
Methods: We identified UC patients that were prescribed Upadacitinib between June 1st , 2022, to February 6th, 2023, within the MedStar Health System. Inclusion criteria included: age >18 years, histological diagnosis of UC, and upadacitinib prescribed and filled at any MedStar Gastroenterology clinic site.
Results: Fifteen patients met the inclusion criteria, 7 females (47%), and 8 males (53%) with a mean age of 33.9 years. The mean disease duration was 7.8 years, and 13 patients had a history of pancolitis, while 2 had proctitis. All patients had been treated with at least one biologic agent in the past and the mean number of biologic agent trials per patient was 2.5. Four patients had tried ozanimod, which was discontinued for various reasons. We assessed baseline disease activity clinically, biochemically, and endoscopically. The mean serum CRP concentration and Fecal Calprotectin levels were 23 mg/L and 1392mg/kg, respectively, and the mean Mayo endoscopic score was 2.1, with two patients having endoscopically quiescent disease (Mayo score=0). Twelve patients returned for follow-up during which their response to treatment was assessed, with 9 patients reporting significant clinical improvement or inactive disease. Two patients had to discontinue upadacitinib due to weight gain/acne and deep venous thrombosis (identified shortly prior to therapy initiation). Mean serum CRP concentration and Fecal Calprotectin levels were 12 mg/L and 271mg/kg, respectively, at follow-up.
Discussion: Our experience demonstrates that upadacitinib is well tolerated and effective in most patients with biologic refractory UC. This is supported by the clinical and biochemical remission observed as well as the minimal side effects reported. Future large-scale population studies are warranted to identify upadacitinib-responsive patients and define long-term remission rates and side effects.

Figure:
Table A: Patient Demographics and Disease Characteristics, Table B: Baseline Disease Activity, Table C: Response to Upadacitinib, Figure D: Serum CRP (mg/L) at baseline and 3-month follow up, Figure E: Fecal Calprotectin (mg/Kg) at baseline and 3-month follow up. Abbreviations: Female (F), Male (M), Body Mass index (BMI), Extra-intestinal Manifestations (EIMs), C-reactive Protein (CRP).
Table A: Patient Demographics and Disease Characteristics, Table B: Baseline Disease Activity, Table C: Response to Upadacitinib, Figure D: Serum CRP (mg/L) at baseline and 3-month follow up, Figure E: Fecal Calprotectin (mg/Kg) at baseline and 3-month follow up. Abbreviations: Female (F), Male (M), Body Mass index (BMI), Extra-intestinal Manifestations (EIMs), C-reactive Protein (CRP).
Disclosures:
Stavros Doumas indicated no relevant financial relationships.
Sophia Dahmani indicated no relevant financial relationships.
Harjit Singh indicated no relevant financial relationships.
Peter Chi indicated no relevant financial relationships.
Mark Mattar indicated no relevant financial relationships.
Stavros Doumas, MD, MSc1, Sophia Dahmani, BSc2, Harjit Singh, MD1, Peter Chi, BSN1, Mark Mattar, MD1. P2138 - Upadacitinib in Ulcerative Colitis: Early Experience From a Large Regional Health System, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
