Monday Poster Session
Category: IBD
P2140 - Fatigue Status and Risk of Inflammatory Bowel Disease: A Longitudinal Cohort Study and Mendelian Randomization Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- LZ
Lijun Zhang, MD
Guangdong Provincial People's Hospital
Guangzhou, Guangdong, China
Presenting Author(s)
Lijun Zhang, MD1, Yuying Ma, MD2, Wentao Huang, MD2, Ruibang Luo, PhD3, Felix W. Leung, MD, FACG4, Chongyang Duan, PhD5, Weihong Sha, PhD2, Hao Chen, PhD2
1Guangdong Provincial People's Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, Guangdong, China; 2Guangdong Provincial People's Hospital, Guangzhou, Guangdong, China; 3University of Hong Kong, HongKong, Hong Kong; 4Sepulveda ACC/VAGLAHS/UCLA, North Hills, CA; 5Southern Medical University, Guangzhou, Guangdong, China
Introduction: Fatigue has garnered significant attention due to its detrimental effects on overall health and well-being. Fatigue was previously considered as a common symptom of Inflammatory Bowel Disease (IBD). However, approximately 50% of patients with IBD have experienced fatigue before their initial diagnosis. Whether fatigue is the cause or result of IBD remains unknown. Thus, this study was to explore the causal association between fatigue and IBD.
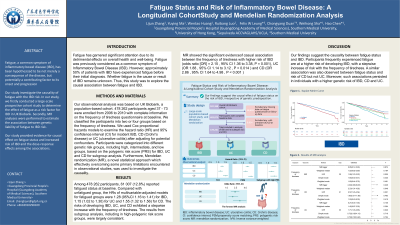
Methods: Our observational analysis was based on UK Biobank, a population-based cohort. 478 262 participants aged 37 - 73 were enrolled from 2006 to 2010 with complete information on the frequency of tiredness questionnaire at baseline. We classified the participants into two or four groups based on the frequency of tiredness. We used Cox proportional hazards models to examine the hazard ratio (HR) and 95% confidence interval (CI) for incident IBD, CD (Crohn's disease) or UC (ulcerative colitis) after adjusting for potential confounders. Participants were categorized into different genetic risk groups, including high, intermediate, and low groups, based on the polygenic risk score (PRS) for IBD, UC and CD for subgroup analysis. Furthermore, Mendelian randomization (MR) study was used to investigate the causality.
Results: Among 478 262 participants, 61 007 (12.8%) reported fatigued status at baseline. Compared with unfatigued group, the HRs of multivariable-adjusted models for fatigued groups were 1.28 (95%CI 1.16 to 1.41) for IBD, 1.15 (1.02 to 1.30) for UC and 1.55 (1.32 to 1.56) for CD. The risks of developing IBD, UC, and CD exhibited a stepwise increase with the frequency of tiredness. The results from subgroup analysis, including in high-polygenic risk score groups, were largely consistent. MR showed the significant evidence of casual association between the frequency of tiredness with higher risk of IBD (odds ratio [OR] = 2.15 , 95% CI 1.36 to 3.38, P = 0.001), UC (OR 1.88 , 95% CI 1.14 to 3.12 , P = 0.014 ) and CD (OR 2.86 , 95% CI 1.64 to 4.98 , P < 0.001 ).
Discussion: Our findings suggest the causality between fatigue status and IBD. Participants frequently experienced fatigue are at a higher risk of developing IBD, with a stepwise increase of risk with the frequency of tiredness. A similar association was also observed between fatigue status and risk of CD but not UC. Moreover, such associations persisted in individuals with a higher genetic risk of IBD, CD and UC.
Disclosures:
Lijun Zhang, MD1, Yuying Ma, MD2, Wentao Huang, MD2, Ruibang Luo, PhD3, Felix W. Leung, MD, FACG4, Chongyang Duan, PhD5, Weihong Sha, PhD2, Hao Chen, PhD2. P2140 - Fatigue Status and Risk of Inflammatory Bowel Disease: A Longitudinal Cohort Study and Mendelian Randomization Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Guangdong Provincial People's Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, Guangdong, China; 2Guangdong Provincial People's Hospital, Guangzhou, Guangdong, China; 3University of Hong Kong, HongKong, Hong Kong; 4Sepulveda ACC/VAGLAHS/UCLA, North Hills, CA; 5Southern Medical University, Guangzhou, Guangdong, China
Introduction: Fatigue has garnered significant attention due to its detrimental effects on overall health and well-being. Fatigue was previously considered as a common symptom of Inflammatory Bowel Disease (IBD). However, approximately 50% of patients with IBD have experienced fatigue before their initial diagnosis. Whether fatigue is the cause or result of IBD remains unknown. Thus, this study was to explore the causal association between fatigue and IBD.
Methods: Our observational analysis was based on UK Biobank, a population-based cohort. 478 262 participants aged 37 - 73 were enrolled from 2006 to 2010 with complete information on the frequency of tiredness questionnaire at baseline. We classified the participants into two or four groups based on the frequency of tiredness. We used Cox proportional hazards models to examine the hazard ratio (HR) and 95% confidence interval (CI) for incident IBD, CD (Crohn's disease) or UC (ulcerative colitis) after adjusting for potential confounders. Participants were categorized into different genetic risk groups, including high, intermediate, and low groups, based on the polygenic risk score (PRS) for IBD, UC and CD for subgroup analysis. Furthermore, Mendelian randomization (MR) study was used to investigate the causality.
Results: Among 478 262 participants, 61 007 (12.8%) reported fatigued status at baseline. Compared with unfatigued group, the HRs of multivariable-adjusted models for fatigued groups were 1.28 (95%CI 1.16 to 1.41) for IBD, 1.15 (1.02 to 1.30) for UC and 1.55 (1.32 to 1.56) for CD. The risks of developing IBD, UC, and CD exhibited a stepwise increase with the frequency of tiredness. The results from subgroup analysis, including in high-polygenic risk score groups, were largely consistent. MR showed the significant evidence of casual association between the frequency of tiredness with higher risk of IBD (odds ratio [OR] = 2.15 , 95% CI 1.36 to 3.38, P = 0.001), UC (OR 1.88 , 95% CI 1.14 to 3.12 , P = 0.014 ) and CD (OR 2.86 , 95% CI 1.64 to 4.98 , P < 0.001 ).
Discussion: Our findings suggest the causality between fatigue status and IBD. Participants frequently experienced fatigue are at a higher risk of developing IBD, with a stepwise increase of risk with the frequency of tiredness. A similar association was also observed between fatigue status and risk of CD but not UC. Moreover, such associations persisted in individuals with a higher genetic risk of IBD, CD and UC.
Disclosures:
Lijun Zhang indicated no relevant financial relationships.
Yuying Ma indicated no relevant financial relationships.
Wentao Huang indicated no relevant financial relationships.
Ruibang Luo indicated no relevant financial relationships.
Felix Leung indicated no relevant financial relationships.
Chongyang Duan indicated no relevant financial relationships.
Weihong Sha indicated no relevant financial relationships.
Hao Chen indicated no relevant financial relationships.
Lijun Zhang, MD1, Yuying Ma, MD2, Wentao Huang, MD2, Ruibang Luo, PhD3, Felix W. Leung, MD, FACG4, Chongyang Duan, PhD5, Weihong Sha, PhD2, Hao Chen, PhD2. P2140 - Fatigue Status and Risk of Inflammatory Bowel Disease: A Longitudinal Cohort Study and Mendelian Randomization Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
