Monday Poster Session
Category: IBD
P2144 - The Role of Anxiety and Depression in Perceived Disability Among Inflammatory Bowel Disease Patients
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Nathan Fakult, BA
Case Western Reserve University School of Medicine
Cleveland, OH
Presenting Author(s)
Jill Knepprath, MD1, Nathan Fakult, BA2, Amanda Quinones, BA2, Emad Mansoor, MD3, Keming Gao, MD, PhD4, Jeffry Katz, MD5
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2Case Western Reserve University School of Medicine, Cleveland, OH; 3Case Western Reserve University / University Hospitals, Cleveland, OH; 4Case Western Reserve University / University Hospitals Cleveland Medical Center, Cleveland, OH; 5Case Western Reserve/UHCMC, Cleveland, OH
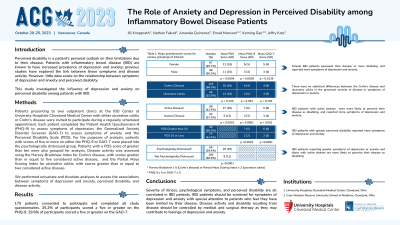
Introduction: Perceived disability is a patient’s personal outlook on their limitations due to their disease. Patients with inflammatory bowel disease (IBD) are known to have increased prevalence of depression and anxiety. The link between psychological symptoms and disease activity in IBD patients has been explored in previous studies. However, there is little data on the relationship between perceived disability and psychological symptoms in IBD patients. The goal of this study was to investigate the influence of depression and anxiety on perceived disability among patients with IBD.
Methods: Patients in two outpatient clinics at the IBD Center at University Hospitals Cleveland Medical Center with ulcerative colitis or Crohn’s disease were invited to participate. Each patient completed the Patient Health Questionnaire-9 (PHQ-9), the Generalized Anxiety Disorder Screener (GAD-7), and the Perceived Disability Scale (PDS). Disease activity was assessed using the Harvey-Bradshaw Index or Partial Mayo Scoring Index. We performed univariate analyses to assess the association between symptoms of depression and anxiety and PDS, as well as disease activity and PDS.
Results: 175 patients consented to participate. The mean age was 49 years old, 50.3% of participants were male, and 68.0% had a diagnosis of Crohn’s disease. Patients with a score of 5 or more in either the PHQ-9 and GAD-7 were placed into the positive psychological symptoms group and those with a score of 4 or less in both were placed in the negative psychological symptoms group. Patients with psychological symptoms had a higher PDS score than those without psychological symptoms (p< 0.0001).
Patients were grouped according to disease activity with a Harvey-Bradshaw Index score of 5 or more or a Partial Mayo Scoring Index score of 2 or more indicating active disease. Patients with active disease had higher PDS, PHQ-9, and GAD-7 scores compared to patients with inactive disease (p< 0.0001, p< 0.0001, and p=0.001, respectively). There was no significant difference in PDS, PHQ-9, and GAD-7 scores between Crohn’s disease and ulcerative colitis patients (Table 1).
Discussion: Based on preliminary data, IBD patients with symptoms of depression or anxiety and with active disease are more likely to perceive their disease as disabling. This emphasizes the importance of screening for depressive/anxious symptoms in this patient population, with special attention to patients who feel they have been limited by their disease.
Disclosures:
Jill Knepprath, MD1, Nathan Fakult, BA2, Amanda Quinones, BA2, Emad Mansoor, MD3, Keming Gao, MD, PhD4, Jeffry Katz, MD5. P2144 - The Role of Anxiety and Depression in Perceived Disability Among Inflammatory Bowel Disease Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2Case Western Reserve University School of Medicine, Cleveland, OH; 3Case Western Reserve University / University Hospitals, Cleveland, OH; 4Case Western Reserve University / University Hospitals Cleveland Medical Center, Cleveland, OH; 5Case Western Reserve/UHCMC, Cleveland, OH
Introduction: Perceived disability is a patient’s personal outlook on their limitations due to their disease. Patients with inflammatory bowel disease (IBD) are known to have increased prevalence of depression and anxiety. The link between psychological symptoms and disease activity in IBD patients has been explored in previous studies. However, there is little data on the relationship between perceived disability and psychological symptoms in IBD patients. The goal of this study was to investigate the influence of depression and anxiety on perceived disability among patients with IBD.
Methods: Patients in two outpatient clinics at the IBD Center at University Hospitals Cleveland Medical Center with ulcerative colitis or Crohn’s disease were invited to participate. Each patient completed the Patient Health Questionnaire-9 (PHQ-9), the Generalized Anxiety Disorder Screener (GAD-7), and the Perceived Disability Scale (PDS). Disease activity was assessed using the Harvey-Bradshaw Index or Partial Mayo Scoring Index. We performed univariate analyses to assess the association between symptoms of depression and anxiety and PDS, as well as disease activity and PDS.
Results: 175 patients consented to participate. The mean age was 49 years old, 50.3% of participants were male, and 68.0% had a diagnosis of Crohn’s disease. Patients with a score of 5 or more in either the PHQ-9 and GAD-7 were placed into the positive psychological symptoms group and those with a score of 4 or less in both were placed in the negative psychological symptoms group. Patients with psychological symptoms had a higher PDS score than those without psychological symptoms (p< 0.0001).
Patients were grouped according to disease activity with a Harvey-Bradshaw Index score of 5 or more or a Partial Mayo Scoring Index score of 2 or more indicating active disease. Patients with active disease had higher PDS, PHQ-9, and GAD-7 scores compared to patients with inactive disease (p< 0.0001, p< 0.0001, and p=0.001, respectively). There was no significant difference in PDS, PHQ-9, and GAD-7 scores between Crohn’s disease and ulcerative colitis patients (Table 1).
Discussion: Based on preliminary data, IBD patients with symptoms of depression or anxiety and with active disease are more likely to perceive their disease as disabling. This emphasizes the importance of screening for depressive/anxious symptoms in this patient population, with special attention to patients who feel they have been limited by their disease.
Disclosures:
Jill Knepprath indicated no relevant financial relationships.
Nathan Fakult indicated no relevant financial relationships.
Amanda Quinones indicated no relevant financial relationships.
Emad Mansoor indicated no relevant financial relationships.
Keming Gao indicated no relevant financial relationships.
Jeffry Katz: Janssen, Pharmaceuticals – Grant/Research Support.
Jill Knepprath, MD1, Nathan Fakult, BA2, Amanda Quinones, BA2, Emad Mansoor, MD3, Keming Gao, MD, PhD4, Jeffry Katz, MD5. P2144 - The Role of Anxiety and Depression in Perceived Disability Among Inflammatory Bowel Disease Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
