Monday Poster Session
Category: IBD
P2148 - Higher Rates of Delay in Starting Advanced Inflammatory Bowel Disease Therapy for Biologics Given via Infusion Centers
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- KX
Karen Xiao, MD
Yale University
New Haven, Connecticut
Presenting Author(s)
Karen Xiao, MD1, Sara Gottesman, MD2, Hang Nguyen, BS1, Elizabeth Hernandez, MD1, Thritha Anand, BS2, Emily Saweris, BS2, Priyanka Jaganathan, MD, MBA2, Faraz Jafri, BS3, Jonathan Davis, BS1, Kimhouy Tong, PharmD4, Jill Gaidos, MD, FACG1, Linda A. Feagins, MD, FACG2
1Yale University, New Haven, CT; 2Dell Medical School at The University of Texas at Austin, Austin, TX; 3Dell Medical School, Austin, TX; 4Yale New Haven Health, New Haven, CT
Introduction: Because biologic and small molecule therapy is expensive, payors have mandated pre-authorization processes for these specialty medications often resulting in a lengthy approval process with delays between prescription and administration of appropriate therapy. The aims of this study are to assess the frequency of and risk factors for delays in starting advanced therapies and to compare patients with and without delays and the effects on IBD-related outcomes.
Methods: Retrospective, multi-center study of adult inflammatory bowel disease (IBD) patients with prescriptions for a biologic or small molecule therapy in one of two academic gastroenterology practices in different regions of the country: the South (Site 1) and the Northeast (Site 2). A priori we defined a delay in starting therapy as more than 14 days between prescription and first dose. Outcomes included days on corticosteroids, IBD-related emergency department (ED) visits, hospitalizations, and surgeries at 3, 6, and 12 months.
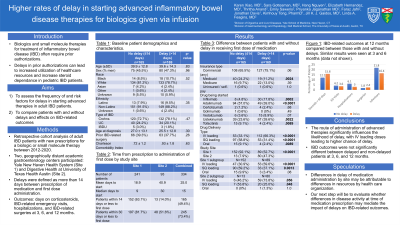
Results: A total of 334 patients (252 Crohn’s disease, 74 ulcerative colitis, 8 IBD undetermined) were prescribed a biologic or small molecule with 49% receiving their first dose within 14 days (mean 25 days, median 15 days). Overall, patients who were on time vs delayed in receiving their first dose were similar regarding age, sex, race, ethnicity, disease type and Charleston Comorbidity Index (CCI) score. Those with delays were less likely to have Medicaid, more likely to be starting a therapy with IV loading (as opposed to SQ or oral), and more likely to be receiving care at the site in the South. On subgroup analysis by study site, delays were more likely in those starting IV therapy at both sites (see table). There were no differences in steroid use, IBD-related ED visits, hospitalizations, or surgeries at 3, 6, or 12 months between groups (see figure).
Discussion: In a cohort of patients from two academic sites, we found that a delay between prescription and administration of first dose of an advanced therapy is common, with over 50% of patients having the first dose delayed more than 2 weeks. Further, we found that a delay in starting therapy was significantly more likely if given via IV induction. This held true on subgroup analysis between sites. We did not find any adverse outcomes from these delays but suspect that we may see a difference for patients who were specifically starting therapy for active disease. Further analyses are underway.

Disclosures:
Karen Xiao, MD1, Sara Gottesman, MD2, Hang Nguyen, BS1, Elizabeth Hernandez, MD1, Thritha Anand, BS2, Emily Saweris, BS2, Priyanka Jaganathan, MD, MBA2, Faraz Jafri, BS3, Jonathan Davis, BS1, Kimhouy Tong, PharmD4, Jill Gaidos, MD, FACG1, Linda A. Feagins, MD, FACG2. P2148 - Higher Rates of Delay in Starting Advanced Inflammatory Bowel Disease Therapy for Biologics Given via Infusion Centers, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Yale University, New Haven, CT; 2Dell Medical School at The University of Texas at Austin, Austin, TX; 3Dell Medical School, Austin, TX; 4Yale New Haven Health, New Haven, CT
Introduction: Because biologic and small molecule therapy is expensive, payors have mandated pre-authorization processes for these specialty medications often resulting in a lengthy approval process with delays between prescription and administration of appropriate therapy. The aims of this study are to assess the frequency of and risk factors for delays in starting advanced therapies and to compare patients with and without delays and the effects on IBD-related outcomes.
Methods: Retrospective, multi-center study of adult inflammatory bowel disease (IBD) patients with prescriptions for a biologic or small molecule therapy in one of two academic gastroenterology practices in different regions of the country: the South (Site 1) and the Northeast (Site 2). A priori we defined a delay in starting therapy as more than 14 days between prescription and first dose. Outcomes included days on corticosteroids, IBD-related emergency department (ED) visits, hospitalizations, and surgeries at 3, 6, and 12 months.
Results: A total of 334 patients (252 Crohn’s disease, 74 ulcerative colitis, 8 IBD undetermined) were prescribed a biologic or small molecule with 49% receiving their first dose within 14 days (mean 25 days, median 15 days). Overall, patients who were on time vs delayed in receiving their first dose were similar regarding age, sex, race, ethnicity, disease type and Charleston Comorbidity Index (CCI) score. Those with delays were less likely to have Medicaid, more likely to be starting a therapy with IV loading (as opposed to SQ or oral), and more likely to be receiving care at the site in the South. On subgroup analysis by study site, delays were more likely in those starting IV therapy at both sites (see table). There were no differences in steroid use, IBD-related ED visits, hospitalizations, or surgeries at 3, 6, or 12 months between groups (see figure).
Discussion: In a cohort of patients from two academic sites, we found that a delay between prescription and administration of first dose of an advanced therapy is common, with over 50% of patients having the first dose delayed more than 2 weeks. Further, we found that a delay in starting therapy was significantly more likely if given via IV induction. This held true on subgroup analysis between sites. We did not find any adverse outcomes from these delays but suspect that we may see a difference for patients who were specifically starting therapy for active disease. Further analyses are underway.

Figure: Outcomes at 3 months after prescribed therapy compared between patients who started therapy on time versus delayed > 14 days. All categories were not significantly different between on time and delayed. Data at 6 months and 12 months was similar.
Disclosures:
Karen Xiao indicated no relevant financial relationships.
Sara Gottesman indicated no relevant financial relationships.
Hang Nguyen indicated no relevant financial relationships.
Elizabeth Hernandez indicated no relevant financial relationships.
Thritha Anand indicated no relevant financial relationships.
Emily Saweris indicated no relevant financial relationships.
Priyanka Jaganathan indicated no relevant financial relationships.
Faraz Jafri indicated no relevant financial relationships.
Jonathan Davis indicated no relevant financial relationships.
Kimhouy Tong indicated no relevant financial relationships.
Jill Gaidos: Abbvie – Advisor or Review Panel Member, Grant/Research Support. Bristol Myers Squibb – Grant/Research Support. Pfizer – Consultant, Grant/Research Support.
Linda A. Feagins: Bristol Myers Squibb – Grant/Research Support. Corevitas – Grant/Research Support. Takeda – Grant/Research Support.
Karen Xiao, MD1, Sara Gottesman, MD2, Hang Nguyen, BS1, Elizabeth Hernandez, MD1, Thritha Anand, BS2, Emily Saweris, BS2, Priyanka Jaganathan, MD, MBA2, Faraz Jafri, BS3, Jonathan Davis, BS1, Kimhouy Tong, PharmD4, Jill Gaidos, MD, FACG1, Linda A. Feagins, MD, FACG2. P2148 - Higher Rates of Delay in Starting Advanced Inflammatory Bowel Disease Therapy for Biologics Given via Infusion Centers, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

