Monday Poster Session
Category: IBD
P2164 - Pouch Outcomes in Patients with Inflammatory Bowel Disease and Ileal Pouch Anal Anastomosis Who Undergo Pelvic Radiation
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Karthik Gnanapandithan, MD, MS
Mayo Clinic Florida
Jacksonville, FL
Presenting Author(s)
Karthik Gnanapandithan, MD, MS1, Fadi H.. Mourad, MD2, Bo Shen, MD, FACG3, Francis A. Farraye, MD, MSc, MACG4, Jana G.. Hashash, MD, MSc, FACG4
1Mayo Clinic Florida, Jacksonville, FL; 2American University of Beirut Medical Center, Ras Beirut, Beyrouth, Lebanon; 3Columbia University Medical Center, New York, NY; 4Mayo Clinic, Jacksonville, FL
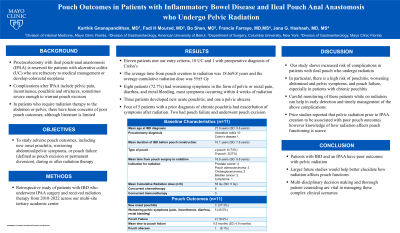
Introduction: Proctocolectomy with ileal pouch-anal anastomosis (IPAA) is a surgical treatment reserved for patients with ulcerative colitis (UC) who are refractory to medical management or develop colorectal neoplasia. Complications after IPAA include pelvic pain, incontinence, pouchitis and strictures, among others. A small subset of patients ultimately require pouch excision. Some patients develop malignancies that require radiation therapy to the lower abdomen or pelvis. There is scarce literature on how radiotherapy affects pouch outcomes, with ongoing concern that it can increase the risk of pouch-related complications.
Methods: Patients with inflammatory bowel disease (IBD) who underwent IPAA surgery and received radiation therapy from 2010-2022 across our multi-site tertiary academic center were included. We assessed adverse pouch outcomes, including new onset pouchitis, worsening abdominal/pelvic symptoms, or pouch failure (defined as pouch excision or permanent diversion), during or after radiation therapy.
Results: Eleven patients met our entry criteria, 10 UC and 1 with preoperative diagnosis of Crohn’s disease. Ten patients received pelvic radiation and 1 abdominal radiation. The average time from pouch creation to radiation was 18.6±9.8 years and the average cumulative radiation dose (when data was available) was 55±5 Gy. Indications for radiation were prostate cancer (4), pouch cancer (2), cholangiocarcinoma (11), bladder cancer (11), and lymphoma (1). Eight patients (72.7%) had worsening symptoms in the form of pelvic or rectal pain, diarrhea, and rectal bleeding. Most patients developed symptoms within 4 weeks of starting radiation. Three patients developed new acute pouchitis after beginning radiation, and one developed a pelvic abscess. Four of 5 patients with a prior diagnosis of chronic pouchitis had exacerbation of symptoms after radiation. Two of those with chronic pouchitis had pouch failure at 6 months and 13 months from the start of radiation and underwent pouch excision. There was no mortality related to radiation therapy.
Discussion: Patients with IBD and an IPAA have poor outcomes with pelvic radiation. In particular, there is a high risk of pouchitis, worsening abdominal and pelvic symptoms, and pouch failure, especially in patients with chronic pouchitis. Multi-disciplinary decision-making and detailed discussion with patients are vital in managing these complex clinical scenarios.
Disclosures:
Karthik Gnanapandithan, MD, MS1, Fadi H.. Mourad, MD2, Bo Shen, MD, FACG3, Francis A. Farraye, MD, MSc, MACG4, Jana G.. Hashash, MD, MSc, FACG4. P2164 - Pouch Outcomes in Patients with Inflammatory Bowel Disease and Ileal Pouch Anal Anastomosis Who Undergo Pelvic Radiation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mayo Clinic Florida, Jacksonville, FL; 2American University of Beirut Medical Center, Ras Beirut, Beyrouth, Lebanon; 3Columbia University Medical Center, New York, NY; 4Mayo Clinic, Jacksonville, FL
Introduction: Proctocolectomy with ileal pouch-anal anastomosis (IPAA) is a surgical treatment reserved for patients with ulcerative colitis (UC) who are refractory to medical management or develop colorectal neoplasia. Complications after IPAA include pelvic pain, incontinence, pouchitis and strictures, among others. A small subset of patients ultimately require pouch excision. Some patients develop malignancies that require radiation therapy to the lower abdomen or pelvis. There is scarce literature on how radiotherapy affects pouch outcomes, with ongoing concern that it can increase the risk of pouch-related complications.
Methods: Patients with inflammatory bowel disease (IBD) who underwent IPAA surgery and received radiation therapy from 2010-2022 across our multi-site tertiary academic center were included. We assessed adverse pouch outcomes, including new onset pouchitis, worsening abdominal/pelvic symptoms, or pouch failure (defined as pouch excision or permanent diversion), during or after radiation therapy.
Results: Eleven patients met our entry criteria, 10 UC and 1 with preoperative diagnosis of Crohn’s disease. Ten patients received pelvic radiation and 1 abdominal radiation. The average time from pouch creation to radiation was 18.6±9.8 years and the average cumulative radiation dose (when data was available) was 55±5 Gy. Indications for radiation were prostate cancer (4), pouch cancer (2), cholangiocarcinoma (11), bladder cancer (11), and lymphoma (1). Eight patients (72.7%) had worsening symptoms in the form of pelvic or rectal pain, diarrhea, and rectal bleeding. Most patients developed symptoms within 4 weeks of starting radiation. Three patients developed new acute pouchitis after beginning radiation, and one developed a pelvic abscess. Four of 5 patients with a prior diagnosis of chronic pouchitis had exacerbation of symptoms after radiation. Two of those with chronic pouchitis had pouch failure at 6 months and 13 months from the start of radiation and underwent pouch excision. There was no mortality related to radiation therapy.
Discussion: Patients with IBD and an IPAA have poor outcomes with pelvic radiation. In particular, there is a high risk of pouchitis, worsening abdominal and pelvic symptoms, and pouch failure, especially in patients with chronic pouchitis. Multi-disciplinary decision-making and detailed discussion with patients are vital in managing these complex clinical scenarios.
Disclosures:
Karthik Gnanapandithan indicated no relevant financial relationships.
Fadi Mourad indicated no relevant financial relationships.
Bo Shen: AbbVie – Consultant. Janssen – Consultant. Takeda – Consultant.
Francis Farraye: AbbVie – Advisory Committee/Board Member. Avalo Therapeutics – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. GSK – Advisory Committee/Board Member. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz Immunology – Advisory Committee/Board Member. Sebela – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Jana Hashash: Iterative Health – Grant/Research Support.
Karthik Gnanapandithan, MD, MS1, Fadi H.. Mourad, MD2, Bo Shen, MD, FACG3, Francis A. Farraye, MD, MSc, MACG4, Jana G.. Hashash, MD, MSc, FACG4. P2164 - Pouch Outcomes in Patients with Inflammatory Bowel Disease and Ileal Pouch Anal Anastomosis Who Undergo Pelvic Radiation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
