Monday Poster Session
Category: IBD
P2181 - Gastrointestinal Adverse Events of Immune Checkpoint Inhibitors in Patients With Inflammatory Bowel Disease: A Multicenter Collaborative Network Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- CN
Chengu Niu, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Chengu Niu, MD1, Kaiwen Zhu, MD1, Jing Zhang, MD2, Tausif Syed, MD1, Muhammad Farhan Ashraf, MD1, Karin Dunnigan, MD1
1Rochester General Hospital, Rochester, NY; 2Rainier Springs Hospital, Vancouver, WA
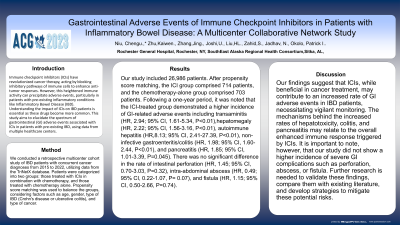
Introduction: Immune checkpoint inhibitors (ICIs) have revolutionized cancer therapy, acting by blocking inhibitory pathways of immune cells to enhance anti-tumor responses. However, this heightened immune activity can precipitate adverse events, particularly in patients with pre-existing inflammatory conditions like Inflammatory Bowel Disease (IBD). Understanding the impact of ICIs on IBD patients is essential as these drugs become more common. This study aims to elucidate the spectrum of gastrointestinal (GI) adverse events associated with ICIs in patients with pre-existing IBD, using data from multiple healthcare centers.
Methods: We conducted a retrospective multicenter cohort study of IBD patients with concurrent GI cancer diagnoses from 2015 to 2022, utilizing data from the TriNetX database. Patients were categorized into two groups: those treated with ICIs in combination with chemotherapy, and those treated with chemotherapy alone. Propensity score matching was used to balance the groups, considering factors such as age, gender, type of IBD (Crohn's disease or ulcerative colitis), and type of cancer.
Results: Our study included 26,986 patients. After propensity score matching, the ICI group comprised 714 patients, and the chemotherapy-alone group comprised 703 patients. Following a one-year period, it was noted that the ICI-treated group demonstrated a higher incidence of GI-related adverse events including transaminitis (HR, 2.94; 95% CI, 1.61-5.34, P< 0.01),hepatomegaly (HR, 2.22; 95% CI, 1.56-3.16, P< 0.01), autoimmune hepatitis (HR,8.13; 95% CI, 2.41-27.39, P< 0.01), non-infective gastroenteritis/colitis (HR, 1.98; 95% CI, 1.60-2.44, P< 0.01), and pancreatitis (HR, 1.85; 95% CI, 1.01-3.39, P=0.045). There was no significant difference in the rate of intestinal perforation (HR, 1.45; 95% CI, 0.70-3.03, P=0.32), intra-abdominal abscess (HR, 0.49; 95% CI, 0.22-1.07, P= 0.07), and fistula (HR, 1.15; 95% CI, 0.50-2.66, P=0.74).
Discussion: Our findings suggest that ICIs, while beneficial in cancer treatment, may contribute to an increased rate of GI adverse events in IBD patients, necessitating vigilant monitoring. The mechanisms behind the increased rates of hepatotoxicity, colitis, and pancreatitis may relate to the overall enhanced immune response triggered by ICIs. It is important to note, however, that our study did not show a higher incidence of severe GI complications such as perforation, abscess, or fistula.
Disclosures:
Chengu Niu, MD1, Kaiwen Zhu, MD1, Jing Zhang, MD2, Tausif Syed, MD1, Muhammad Farhan Ashraf, MD1, Karin Dunnigan, MD1. P2181 - Gastrointestinal Adverse Events of Immune Checkpoint Inhibitors in Patients With Inflammatory Bowel Disease: A Multicenter Collaborative Network Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Rainier Springs Hospital, Vancouver, WA
Introduction: Immune checkpoint inhibitors (ICIs) have revolutionized cancer therapy, acting by blocking inhibitory pathways of immune cells to enhance anti-tumor responses. However, this heightened immune activity can precipitate adverse events, particularly in patients with pre-existing inflammatory conditions like Inflammatory Bowel Disease (IBD). Understanding the impact of ICIs on IBD patients is essential as these drugs become more common. This study aims to elucidate the spectrum of gastrointestinal (GI) adverse events associated with ICIs in patients with pre-existing IBD, using data from multiple healthcare centers.
Methods: We conducted a retrospective multicenter cohort study of IBD patients with concurrent GI cancer diagnoses from 2015 to 2022, utilizing data from the TriNetX database. Patients were categorized into two groups: those treated with ICIs in combination with chemotherapy, and those treated with chemotherapy alone. Propensity score matching was used to balance the groups, considering factors such as age, gender, type of IBD (Crohn's disease or ulcerative colitis), and type of cancer.
Results: Our study included 26,986 patients. After propensity score matching, the ICI group comprised 714 patients, and the chemotherapy-alone group comprised 703 patients. Following a one-year period, it was noted that the ICI-treated group demonstrated a higher incidence of GI-related adverse events including transaminitis (HR, 2.94; 95% CI, 1.61-5.34, P< 0.01),hepatomegaly (HR, 2.22; 95% CI, 1.56-3.16, P< 0.01), autoimmune hepatitis (HR,8.13; 95% CI, 2.41-27.39, P< 0.01), non-infective gastroenteritis/colitis (HR, 1.98; 95% CI, 1.60-2.44, P< 0.01), and pancreatitis (HR, 1.85; 95% CI, 1.01-3.39, P=0.045). There was no significant difference in the rate of intestinal perforation (HR, 1.45; 95% CI, 0.70-3.03, P=0.32), intra-abdominal abscess (HR, 0.49; 95% CI, 0.22-1.07, P= 0.07), and fistula (HR, 1.15; 95% CI, 0.50-2.66, P=0.74).
Discussion: Our findings suggest that ICIs, while beneficial in cancer treatment, may contribute to an increased rate of GI adverse events in IBD patients, necessitating vigilant monitoring. The mechanisms behind the increased rates of hepatotoxicity, colitis, and pancreatitis may relate to the overall enhanced immune response triggered by ICIs. It is important to note, however, that our study did not show a higher incidence of severe GI complications such as perforation, abscess, or fistula.
Disclosures:
Chengu Niu indicated no relevant financial relationships.
Kaiwen Zhu indicated no relevant financial relationships.
Jing Zhang indicated no relevant financial relationships.
Tausif Syed indicated no relevant financial relationships.
Muhammad Farhan Ashraf indicated no relevant financial relationships.
Karin Dunnigan indicated no relevant financial relationships.
Chengu Niu, MD1, Kaiwen Zhu, MD1, Jing Zhang, MD2, Tausif Syed, MD1, Muhammad Farhan Ashraf, MD1, Karin Dunnigan, MD1. P2181 - Gastrointestinal Adverse Events of Immune Checkpoint Inhibitors in Patients With Inflammatory Bowel Disease: A Multicenter Collaborative Network Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
