Monday Poster Session
Category: IBD
P2199 - Guselkumab Improves Health-Related Quality of Life in Patients With Moderately to Severely Active Ulcerative Colitis: Results From the QUASAR Phase 3 Induction Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
- BB
Brian Bressler, MD, MS, FRCPC
St. Paul’s Hospital
Vancouver, British Columbia, Canada
Presenting Author(s)
Brian Bressler, MD, MS, FRCPC1, Brian G. Feagan, MD2, Julian Panés, MD, PhD3, Gary R. Lichtenstein, MD4, Kuan-Hsiang G. Huang, MD, PhD5, Matthew Germinaro, MD5, Dwiti Pandya, MS5, Chenglong Han, MD, PhD6, Ye Miao, MS5, Hongyan Zhang, PhD5, Syed Lateef, MD7, Rima Petroniene, MD, PhD8, Yaser Rayyan, MD9, Laurent Peyrin-Biroulet, MD, PhD10, David T. Rubin, MD, FACG11, Tadakazu Hisamatsu, MD, PhD12
1St. Paul’s Hospital, Vancouver, BC, Canada; 2Western University, London, ON, Canada; 3Hospital Clínic de Barcelona, IDIBAPS, CIBERehd, Barcelona, Catalonia, Spain; 4University of Pennsylvania, Philadelphia, PA; 5Janssen Research & Development, LLC, Spring House, PA; 6Janssen Global Services, LLC, Malvern, PA; 7Gastro Health, Kissimmee, FL; 8Barrie GI Associates, Barrie, ON, Canada; 9University of Jordan, Amman, 'Amman, Jordan; 10Last Inserm U954 and CHU de Nancy, Lorraine University, Vandoeuvre-lès-Nancy, Lorraine, France; 11University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 12Kyorin University School of Medicine, Tokyo, Tokyo, Japan
Introduction: The QUASAR Phase 3 Induction Study assessed the efficacy and safety of guselkumab (GUS), an IL-23 p19 subunit antagonist, as IV induction therapy in adults with moderately to severely active ulcerative colitis (UC) with an inadequate response or intolerance to conventional and/or advanced therapies (ie, TNFα antagonists, integrin receptor antagonists, or Janus kinase inhibitors). Primary outcomes were reported previously; here we report the impact of GUS vs placebo (PBO) on health-related quality of life (HRQoL) at Week (Wk) 12 as measured by the Inflammatory Bowel Disease Questionnaire (IBDQ).
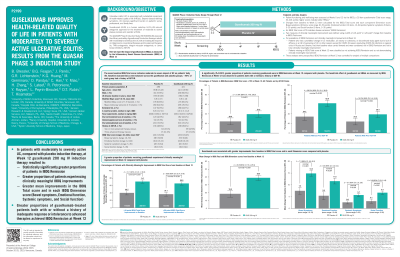
Methods: Patients randomly received in a blinded fashion (3:2) treatment with IV GUS 200mg or PBO at Wks 0/4/8. The primary analysis population included treated patients with a baseline modified Mayo score of 5–9 and an endoscopy subscore ≥2. The IBDQ (Total score range, 32–224) was evaluated at Wks 0/12; higher scores indicate better HRQoL, with a score ≥170 indicating disease remission (IBDQ Remission). Clinically meaningful improvements were defined using cutoffs of ≥16- or > 20-point change from baseline in IBDQ Total score. These analyses were prespecified; only IBDQ Remission at Wk 12 was controlled for analysis of multiple comparisons.
Results: Seven hundred one patients were included in the primary analysis (mean age, 40.5y; male, 56.9%; mean UC duration, 7.5y; mean modified Mayo score, 6.9; Mayo endoscopy subscore of 3, 67.9%). Baseline characteristics were balanced across the GUS and PBO groups; ~49% of each group had a prior inadequate response or intolerance to advanced therapies (ADT-IR). Mean baseline IBDQ Total scores were 125.8 and 126.3 for GUS and PBO, respectively.
Compared with PBO at Wk 12, GUS was associated with greater mean reductions in IBDQ Total and each Dimension score (Bowel, Emotional, Systemic, Social; Table). A significantly greater (p< 0.001) proportion of patients receiving GUS were in IBDQ Remission at Wk 12 vs PBO (51.3% vs 29.6%; adjusted treatment difference, 21.9%). The effect of GUS on IBDQ Remission was also observed in patients with or without prior ADT-IR (Table). A greater proportion of GUS patients achieved clinically meaningful improvements (both IBDQ improvement definitions; Figure).
Discussion: In patients with moderately to severely active UC, induction therapy with IV GUS 200mg resulted in higher rates of clinically meaningful IBDQ improvements and IBDQ Remission at Wk 12 vs PBO. Greater improvements were noted in each of the IBDQ domains.

Disclosures:
Brian Bressler, MD, MS, FRCPC1, Brian G. Feagan, MD2, Julian Panés, MD, PhD3, Gary R. Lichtenstein, MD4, Kuan-Hsiang G. Huang, MD, PhD5, Matthew Germinaro, MD5, Dwiti Pandya, MS5, Chenglong Han, MD, PhD6, Ye Miao, MS5, Hongyan Zhang, PhD5, Syed Lateef, MD7, Rima Petroniene, MD, PhD8, Yaser Rayyan, MD9, Laurent Peyrin-Biroulet, MD, PhD10, David T. Rubin, MD, FACG11, Tadakazu Hisamatsu, MD, PhD12. P2199 - Guselkumab Improves Health-Related Quality of Life in Patients With Moderately to Severely Active Ulcerative Colitis: Results From the QUASAR Phase 3 Induction Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1St. Paul’s Hospital, Vancouver, BC, Canada; 2Western University, London, ON, Canada; 3Hospital Clínic de Barcelona, IDIBAPS, CIBERehd, Barcelona, Catalonia, Spain; 4University of Pennsylvania, Philadelphia, PA; 5Janssen Research & Development, LLC, Spring House, PA; 6Janssen Global Services, LLC, Malvern, PA; 7Gastro Health, Kissimmee, FL; 8Barrie GI Associates, Barrie, ON, Canada; 9University of Jordan, Amman, 'Amman, Jordan; 10Last Inserm U954 and CHU de Nancy, Lorraine University, Vandoeuvre-lès-Nancy, Lorraine, France; 11University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 12Kyorin University School of Medicine, Tokyo, Tokyo, Japan
Introduction: The QUASAR Phase 3 Induction Study assessed the efficacy and safety of guselkumab (GUS), an IL-23 p19 subunit antagonist, as IV induction therapy in adults with moderately to severely active ulcerative colitis (UC) with an inadequate response or intolerance to conventional and/or advanced therapies (ie, TNFα antagonists, integrin receptor antagonists, or Janus kinase inhibitors). Primary outcomes were reported previously; here we report the impact of GUS vs placebo (PBO) on health-related quality of life (HRQoL) at Week (Wk) 12 as measured by the Inflammatory Bowel Disease Questionnaire (IBDQ).
Methods: Patients randomly received in a blinded fashion (3:2) treatment with IV GUS 200mg or PBO at Wks 0/4/8. The primary analysis population included treated patients with a baseline modified Mayo score of 5–9 and an endoscopy subscore ≥2. The IBDQ (Total score range, 32–224) was evaluated at Wks 0/12; higher scores indicate better HRQoL, with a score ≥170 indicating disease remission (IBDQ Remission). Clinically meaningful improvements were defined using cutoffs of ≥16- or > 20-point change from baseline in IBDQ Total score. These analyses were prespecified; only IBDQ Remission at Wk 12 was controlled for analysis of multiple comparisons.
Results: Seven hundred one patients were included in the primary analysis (mean age, 40.5y; male, 56.9%; mean UC duration, 7.5y; mean modified Mayo score, 6.9; Mayo endoscopy subscore of 3, 67.9%). Baseline characteristics were balanced across the GUS and PBO groups; ~49% of each group had a prior inadequate response or intolerance to advanced therapies (ADT-IR). Mean baseline IBDQ Total scores were 125.8 and 126.3 for GUS and PBO, respectively.
Compared with PBO at Wk 12, GUS was associated with greater mean reductions in IBDQ Total and each Dimension score (Bowel, Emotional, Systemic, Social; Table). A significantly greater (p< 0.001) proportion of patients receiving GUS were in IBDQ Remission at Wk 12 vs PBO (51.3% vs 29.6%; adjusted treatment difference, 21.9%). The effect of GUS on IBDQ Remission was also observed in patients with or without prior ADT-IR (Table). A greater proportion of GUS patients achieved clinically meaningful improvements (both IBDQ improvement definitions; Figure).
Discussion: In patients with moderately to severely active UC, induction therapy with IV GUS 200mg resulted in higher rates of clinically meaningful IBDQ improvements and IBDQ Remission at Wk 12 vs PBO. Greater improvements were noted in each of the IBDQ domains.

Figure: Percentage of patients with ≥16- or >20-point IBDQ Total score improvements at Wk 12
Disclosures:
Brian Bressler: AbbVie – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Alimentiv – Advisory Committee/Board Member. Allergan – Advisory Committee/Board Member. Alvine – Grant/Research Support. Amgen – Advisory Committee/Board Member, Grant/Research Support. AMT – Advisory Committee/Board Member. Bausch Health – Advisory Committee/Board Member. Boehringer Ingelheim – Grant/Research Support. Bristol Myers Squibb – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Celgene – Advisory Committee/Board Member, Grant/Research Support. Ferring – Advisory Committee/Board Member, Speakers Bureau. Fresenius Kabi – Advisory Committee/Board Member. Genentech – Advisory Committee/Board Member, Grant/Research Support. Gilead – Advisory Committee/Board Member. GlaxoSmithKline – Grant/Research Support. Iterative Scopes – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Merck – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Microbiome Insights – Advisory Committee/Board Member. Mylan – Advisory Committee/Board Member. Novartis – Advisory Committee/Board Member, Speakers Bureau. Pendopharm – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member, Speakers Bureau. Protagonist – Advisory Committee/Board Member. Qu Biologic – Grant/Research Support, Stock Options. Takeda – Advisory Committee/Board Member, Speakers Bureau.
Brian Feagan: AbbVie – Advisory Committee/Board Member, Consultant, Speakers Bureau. AbolerIS – Consultant. AgomAB Therapeutics – Consultant. Allianthera – Consultant. Amgen – Advisory Committee/Board Member, Consultant. AnaptysBio – Consultant. Applied Molecular Transport Inc. – Consultant. Arena Pharma – Consultant. Avir – Consultant. Azora Therapeutics – Consultant. Baxter – Consultant. BioJamp – Consultant. Biora Therapeutics – Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant. Boston Pharma – Consultant. Bristol Myers Squibb – Consultant. Celgene/BMS – Advisory Committee/Board Member, Consultant. Connect BioPharma – Consultant. Cytoki – Consultant. Disc Medicine – Consultant. Duality – Consultant. EcoR1 – Advisory Committee/Board Member, Consultant. Eli Lilly – Consultant. Equillium – Consultant. Ermium – Consultant. Everest Clinical Research Corp. – Consultant. Ferring Pharmaceuticals – Consultant. First Wave – Consultant. Galapagos – Consultant. Galen Atlantica – Consultant. Genentech/Roche – Advisory Committee/Board Member, Consultant. Gilead – Consultant. GlaxoSmithKline – Advisory Committee/Board Member, Consultant. Glenmark – Consultant. Gossamer Pharma – Consultant, stock shareholder. Hoffmann-LaRoche – Consultant. Hot Spot Therapeutics – Consultant. Imhotex – Consultant. ImmunExt – Consultant. Immunic Therapeutics – Consultant. Index Pharma – Advisory Committee/Board Member, Consultant. Intact Therapeutics – Consultant. JAKAcademy – Consultant. Janssen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Japan Tobacco Inc. – Consultant. Kaleido Biosciences – Consultant. L.E.K. Consulting – Consultant. Landos Biopharma – Consultant. Leadiant – Consultant. LifeSci Capital – Consultant. Lument AB – Consultant. Millennium – Consultant. MiroBio – Consultant. Morphic Therapeutics – Advisory Committee/Board Member, Consultant. Mylan – Consultant. Novartis – Advisory Committee/Board Member. OM Pharma – Consultant. Origo BioPharma – Advisory Committee/Board Member, Consultant. Orphagen – Consultant. Otsuka – Consultant. Pandion Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant. Play to Know AG – Consultant. Progenity – Advisory Committee/Board Member, Consultant. Prometheus Therapeutics and Diagnostics – Advisory Committee/Board Member, Consultant. Protagonist – Consultant. PTM Therapeutics – Consultant. Q32 Bio – Consultant. Rebiotix – Consultant. RedHill Biopharma – Consultant. Redx – Consultant. Roche – Consultant. Sandoz – Consultant. Sanofi – Consultant. Seres Therapeutics – Consultant. Silverback Therapeutics – Consultant. Surrozen Inc. – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau. Teva – Advisory Committee/Board Member, Consultant. Thelium – Consultant. Theravance – Consultant. Tigenix – Consultant. Tillotts Pharma – Advisory Committee/Board Member, Consultant. UCB Pharma – Consultant. VHSquared Ltd. – Consultant. Viatris – Consultant. Western University, Alimentiv Inc – Employee. Ysios – Consultant. Ysopia – Consultant. Zealand Pharma – Consultant.
Julian Panés: AbbVie – Grant/Research Support, Personal fees. Arena – Consultant. Athos – Consultant. Atomwise – Consultant. Boehringer Ingelheim – Consultant. Celgene – Consultant. Celltrion – Consultant. Ferring – Consultant, Speakers Bureau. Galapagos – Consultant. Genentech/Roche – Consultant. GlaxoSmithKline – Consultant. Immunic – Personal fees. Janssen – Consultant, payment for development of educational presentations. Mirum – Consultant. Morphic – Consultant. Origo – Consultant. Pandion – Consultant. Pfizer Inc – Grant/Research Support, payment for development of educational presentations. Progenity – Consultant. Revolo – Consultant. Takeda – payment for development of educational presentations. Theravance – Consultant. Wasserman – Consultant.
Gary R. Lichtenstein: Abbvie – Consultant. American College of Gastroenterology – Honorarium for Associate Editor of American Journal of Gastroenterology. American Gastroenterological Association – CME. American Regent – Consultant, Honorarium [CME Program]. Celgene – Consultant, Grant/Research Support. CellCeutrix – Consultant. Chemed – CME. Eli Lilly – Consultant, Data Safety Monitoring Board. Endo Pharmaceuticals – Consultant. Ferring – Consultant. Gastroenterology and Hepatology – Gastro-Hep Communication, Editor-Honorarium. Gilead – Consultant. IMEDEX – CME. Ironwood – CME. Janssen/ Janssen Orthobiotech – Consultant, Grant/Research Support, Funding to University of PA [IBD Fellow Education]. MedEd Consultants – Consultant. Merck – Consultant, Honorarium [CME Program]. Morphic Therapeutics – Consultant. Pfizer Pharmaceuticals – Consultant, Funding to University of PA [IBD Fellow Education]. Professional Communications, Inc – Royalty for writing Textbook. Prometheus Laboratories, Inc – Consultant. Romark – Consultant, Honorarium for CME. Salix Pharmaceuticals/Valeant – Consultant. Sandoz – Consultant. Shire Pharmaceuticals – Consultant. SLACK, Inc – Book Royalty. Springer Science and Business Media – Editor [Honorarium]. Takeda – Consultant, Grant/Research Support, Funding to University of PA [IBD Fellow Education]. UCB – Consultant, Grant/Research Support. University of Kentucky – CME. Up-To-Date – Author [Honorarium]. Vindico – CME. Virgo – Consultant, Stock Options.
Kuan-Hsiang G. Huang: Johnson & Johnson – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Matthew Germinaro: Johnson & Johnson – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Dwiti Pandya: Janssen – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Chenglong Han: Johnson & Johnson – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Ye Miao: Johnson & Johnson – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Hongyan Zhang: Johnson & Johnson – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Syed Lateef: Janssen – Grant/Research Support.
Rima Petroniene: Janssen – Grant/Research Support. Takeda – Grant/Research Support.
Yaser Rayyan: Janssen – Grant/Research Support.
Laurent Peyrin-Biroulet: AbbVie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Allergan – personal fees. Alma – personal fees. Amgen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Applied Molecular Transport – personal fees. Arena – personal fees. Biogaran – Advisory Committee/Board Member, Consultant, Speakers Bureau. Biogen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant, Speakers Bureau. Bristol Myers Squibb – personal fees. Celgene – Advisory Committee/Board Member, Consultant, Speakers Bureau. Celltrion – Advisory Committee/Board Member, Consultant, Speakers Bureau. CTMA – Stock Options. Eli Lilly – Advisory Committee/Board Member, Consultant, Speakers Bureau. Enterome – personal fees. Enthera – personal fees. Ferring – Advisory Committee/Board Member, Consultant, Speakers Bureau. Forward Pharma – Advisory Committee/Board Member, Consultant, Speakers Bureau. Fresenius – personal fees. Genentech – Advisory Committee/Board Member, Consultant, Speakers Bureau. Gilead – personal fees. H.A.C. Pharma – Advisory Committee/Board Member, Consultant, Speakers Bureau. Hikma – personal fees. Hospira/Pfizer – Advisory Committee/Board Member, Consultant, Speakers Bureau. Index Pharmaceuticals – Advisory Committee/Board Member, Consultant, Speakers Bureau. Janssen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Lycera – Advisory Committee/Board Member, Consultant, Speakers Bureau. Merck – Advisory Committee/Board Member, Consultant, Speakers Bureau. Mitsubishi – Advisory Committee/Board Member, Consultant, Speakers Bureau. MSD – Grant/Research Support, personal fees. Mylan – personal fees. Nestlé – personal fees. Norgine – Advisory Committee/Board Member, Consultant, Speakers Bureau. Oppilan Pharma – personal fees. OSE Immunotherapeutics – personal fees. Pfizer – personal fees. Pharmacosmos – personal fees. Roche – personal fees. Samsung Bioepis – Advisory Committee/Board Member, Consultant, Speakers Bureau. Sandoz – Advisory Committee/Board Member, Consultant, Speakers Bureau. Sterna – personal fees. Sublimity Therapeutics – personal fees. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau. Theravance – Advisory Committee/Board Member, Consultant, Speakers Bureau. Tillots – Advisory Committee/Board Member, Consultant, Speakers Bureau. Vifor – Advisory Committee/Board Member, Consultant, Speakers Bureau.
David T. Rubin: AbbVie – Consultant. Alike Health – Stock Options. AltruBio – Consultant, Stock Options. Aslan Pharmaceuticals – Consultant. Athos Therapeutics – Consultant. Bellatrix Pharmaceuticals – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Celgene – Consultant. Chronicles – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Advisory Committee/Board Member. Crohn's & Colitis Foundation – Advisory Committee/Board Member. Datos Health – Stock Options. EcoR1 – Consultant. Eli Lilly – Consultant. GastroIntestinal Research Foundation – Grant/Research Support. Genentech/Roche – Consultant. Gilead Sciences – Consultant. Helmsley Charitable Trust – Grant/Research Support. Iterative Health – Consultant. Iterative Health – Stock Options. Janssen – Consultant. Kaleido Biosciences – Consultant. Pfizer – Consultant. Prometheus Biosciences – Consultant. Reistone – Consultant. Seres Therapeutics – Consultant. Syneos – Consultant. Takeda – Consultant, Grant/Research Support. Target RWE – Consultant. Trellus Health – Consultant.
Tadakazu Hisamatsu: AbbVie GK – Grant/Research Support, honoraria and had expenses paid to attend or give a presentation/advice at a meeting. Alfresa Pharma Corporation and EA Pharma Co., Ltd – Grant/Research Support. Daiichi-Sankyo – Grant/Research Support. EA Pharma Co, Ltd – Grant/Research Support, honoraria and had expenses paid to attend or give a presentation/advice at a meeting. Eli Lilly – Consultant. Gilead Sciences – honoraria and had expenses paid to attend or give a presentation/advice at a meeting. Janssen Pharmaceutical K.K. – honoraria and had expenses paid to attend or give a presentation/advice at a meeting. JIMRO Co., Ltd – Grant/Research Support, honoraria and had expenses paid to attend or give a presentation/advice at a meeting. KISSEI PHARMACEUTICAL CO., LTD – honoraria and had expenses paid to attend or give a presentation/advice at a meeting. Kyorin Pharmaceutical Co., Ltd – Grant/Research Support, honoraria and had expenses paid to attend or give a presentation/advice at a meeting. Mitsubishi Tanabe Pharma Corporation – Grant/Research Support, honoraria and had expenses paid to attend or give a presentation/advice at a meeting. Mochida Pharmacuetical Co., Ltd – Grant/Research Support, honoraria and had expenses paid to attend or give a presentation/advice at a meeting. Nichi-Iko Pharmaceutical Co., Ltd – honoraria and had expenses paid to attend or give a presentation/advice at a meeting. Nippon Kayaku Co., Ltd – Grant/Research Support. Pfizer Japan Inc. – Grant/Research Support, honoraria and had expenses paid to attend or give a presentation/advice at a meeting. Takeda Pharmaceutical Co., Ltd – Grant/Research Support, honoraria and had expenses paid to attend or give a presentation/advice at a meeting. Zeria Pharmaceutical Co., Ltd – Grant/Research Support.
Brian Bressler, MD, MS, FRCPC1, Brian G. Feagan, MD2, Julian Panés, MD, PhD3, Gary R. Lichtenstein, MD4, Kuan-Hsiang G. Huang, MD, PhD5, Matthew Germinaro, MD5, Dwiti Pandya, MS5, Chenglong Han, MD, PhD6, Ye Miao, MS5, Hongyan Zhang, PhD5, Syed Lateef, MD7, Rima Petroniene, MD, PhD8, Yaser Rayyan, MD9, Laurent Peyrin-Biroulet, MD, PhD10, David T. Rubin, MD, FACG11, Tadakazu Hisamatsu, MD, PhD12. P2199 - Guselkumab Improves Health-Related Quality of Life in Patients With Moderately to Severely Active Ulcerative Colitis: Results From the QUASAR Phase 3 Induction Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
