Monday Poster Session
Category: IBD
P2205 - Sustained Improvement in Inflammatory Bowel Disease Questionnaire Outcomes in Moderately to Severely Active Ulcerative Colitis with Continued Mirikizumab Treatment in Phase 3 LUCENT-3 Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Bruce E. Sands, MD, MS, FACG
Icahn School of Medicine at Mount Sinai
New York, New York
Presenting Author(s)
Bruce E. Sands, MD, MS, FACG1, Brian G. Feagan, MD2, Alessandro Armuzzi, MD, PhD3, Kim McGinnis, CPNP4, Keisa Lynch, DNP, APRN, FNP5, Theresa Hunter Gibble, PhD, MPH4, Jordan Johns, PhD4, Corey A. Siegel, MD, MS6, Vipul Jairath, MBChB, DPhil2
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Western University, London, ON, Canada; 3IBD Center, IRCCS Humanitas Research Hospital, Rozzano (Milan); Department of Biomedical Sciences, Humanitas University, Pieve Emanuele (Milan), Milan, Lombardia, Italy; 4Eli Lilly and Company, Indianapolis, IN; 5University of Utah School of Medicine, Salt Lake City, UT; 6Dartmouth-Hitchcock Inflammatory Bowel Disease Center, Dartmouth-Hitchcock Medical Center, Lebanon, NH
Introduction: Mirikizumab (miri) significantly improved quality of life as evidenced by the Inflammatory Bowel Disease Questionnaire (IBDQ) scores in moderately to severely active ulcerative colitis (UC) during 12-week (W) induction (LUCENT-1) and 40-W maintenance (LUCENT-2) phase 3 studies.1 IBDQ response and remission rates were significantly higher with miri versus placebo in both studies.1 Here we report interim results of 104-W of continuous miri therapy on IBDQ outcomes from an ongoing open-label, single-arm, phase 3, multicenter, long-term extension study (LUCENT-3/NCT03519945).
Methods: Patients who completed LUCENT-2 and achieved clinical response or remission after 52-W of continuous miri therapy entered LUCENT-3 and continued to receive miri 200 mg every 4 weeks subcutaneously. Least squares mean change from baseline in IBDQ total and domain scores were evaluated at W104 using an analysis of covariance model. IBDQ response (≥16-point improvement from baseline)1 and IBDQ remission (IBDQ total score ≥170)1 rates, stratified by prior biologic failure status, were assessed at W104. Missing data were imputed using modified baseline observation carried forward (IBDQ change from baseline) and non-responder imputation (IBDQ response and remission rates).
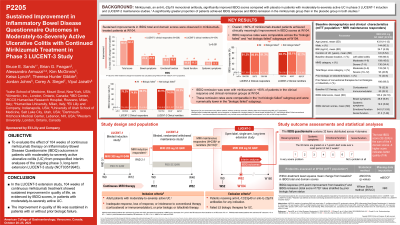
Results: Among the 239 patients with clinical response at W52 who entered the LUCENT-3 study, 154 were in clinical remission. Improvements in IBDQ total and domain scores for these patients were sustained at W104 (Figure 1A). IBDQ response at W104 was seen in over 80% of patients and was comparable across ‘biologic failed’ and ‘not biologic failed’ subgroups (Figure 1B). IBDQ remission rates in the clinical response (78.2%) and clinical remission (80.5%) groups were sustained in ‘not biologic failed’ subgroup (80.1% and 83.2%) and were numerically lower in ‘biologic failed’ subgroup (74.0% and 74.5%), respectively (Figure 1C).
Discussion: In the LUCENT-3 extension study, treatment with mirikizumab showed sustained improvement in quality of life up to W104 in patients with moderately to severely active UC with or without prior biologic failure.
1Sands BE, et al. Mirikizumab improves quality of life in moderately to severely active ulcerative colitis: improvement in inflammatory bowel disease scores in participants of the LUCENT-1 and LUCENT-2 randomized, double-blind, placebo-controlled phase 3 induction and maintenance trials. United European Gastroenterol J. 2022;10(S8):778.

Disclosures:
Bruce E. Sands, MD, MS, FACG1, Brian G. Feagan, MD2, Alessandro Armuzzi, MD, PhD3, Kim McGinnis, CPNP4, Keisa Lynch, DNP, APRN, FNP5, Theresa Hunter Gibble, PhD, MPH4, Jordan Johns, PhD4, Corey A. Siegel, MD, MS6, Vipul Jairath, MBChB, DPhil2. P2205 - Sustained Improvement in Inflammatory Bowel Disease Questionnaire Outcomes in Moderately to Severely Active Ulcerative Colitis with Continued Mirikizumab Treatment in Phase 3 LUCENT-3 Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Western University, London, ON, Canada; 3IBD Center, IRCCS Humanitas Research Hospital, Rozzano (Milan); Department of Biomedical Sciences, Humanitas University, Pieve Emanuele (Milan), Milan, Lombardia, Italy; 4Eli Lilly and Company, Indianapolis, IN; 5University of Utah School of Medicine, Salt Lake City, UT; 6Dartmouth-Hitchcock Inflammatory Bowel Disease Center, Dartmouth-Hitchcock Medical Center, Lebanon, NH
Introduction: Mirikizumab (miri) significantly improved quality of life as evidenced by the Inflammatory Bowel Disease Questionnaire (IBDQ) scores in moderately to severely active ulcerative colitis (UC) during 12-week (W) induction (LUCENT-1) and 40-W maintenance (LUCENT-2) phase 3 studies.1 IBDQ response and remission rates were significantly higher with miri versus placebo in both studies.1 Here we report interim results of 104-W of continuous miri therapy on IBDQ outcomes from an ongoing open-label, single-arm, phase 3, multicenter, long-term extension study (LUCENT-3/NCT03519945).
Methods: Patients who completed LUCENT-2 and achieved clinical response or remission after 52-W of continuous miri therapy entered LUCENT-3 and continued to receive miri 200 mg every 4 weeks subcutaneously. Least squares mean change from baseline in IBDQ total and domain scores were evaluated at W104 using an analysis of covariance model. IBDQ response (≥16-point improvement from baseline)1 and IBDQ remission (IBDQ total score ≥170)1 rates, stratified by prior biologic failure status, were assessed at W104. Missing data were imputed using modified baseline observation carried forward (IBDQ change from baseline) and non-responder imputation (IBDQ response and remission rates).
Results: Among the 239 patients with clinical response at W52 who entered the LUCENT-3 study, 154 were in clinical remission. Improvements in IBDQ total and domain scores for these patients were sustained at W104 (Figure 1A). IBDQ response at W104 was seen in over 80% of patients and was comparable across ‘biologic failed’ and ‘not biologic failed’ subgroups (Figure 1B). IBDQ remission rates in the clinical response (78.2%) and clinical remission (80.5%) groups were sustained in ‘not biologic failed’ subgroup (80.1% and 83.2%) and were numerically lower in ‘biologic failed’ subgroup (74.0% and 74.5%), respectively (Figure 1C).
Discussion: In the LUCENT-3 extension study, treatment with mirikizumab showed sustained improvement in quality of life up to W104 in patients with moderately to severely active UC with or without prior biologic failure.
1Sands BE, et al. Mirikizumab improves quality of life in moderately to severely active ulcerative colitis: improvement in inflammatory bowel disease scores in participants of the LUCENT-1 and LUCENT-2 randomized, double-blind, placebo-controlled phase 3 induction and maintenance trials. United European Gastroenterol J. 2022;10(S8):778.

Figure: Figure 1: IBDQ outcomes at W104 of continuous mirikizumab treatment in patients who achieved clinical responsea or remissionb in LUCENT-2 – mITT population : A) LS mean change from baseline in IBDQ total and domain scores (ANCOVA with mBOCF) ; B) IBDQ response rates (≥16-point improvement from baseline) (NRI); and C) IBDQ remission rates (IBDQ total score ≥170) (NRI)
Baseline was defined as the last nonmissing assessment recorded on or prior to the date of the first study drug administration at Week 0 in LUCENT-1 induction study.
*Within-treatment change from baseline p<0.001 calculated using ANCOVA.
aClinical Responders: Patients who achieved ≥2 points and ≥30% decrease from baseline in MMS and a decrease of ≥1 point in the RB subscore from baseline or an RB score of 0 or 1.
bClinical Remitters: Patients who achieved SF subscore = 0 or 1 with ≥1 point decrease from baseline; RB = 0; ES = 0 or 1.
cBiologic failed: Inadequate response, loss of response, or intolerant to a biologic therapy or Janus kinase inhibitors for UC.
dNot biologic failed: Failed conventional treatments (i.e., immunomodulators/corticosteroids); may include some participants who were exposed to but did not fail biologic treatment.
ANCOVA, analysis of covariance; ES, endoscopic subscore; IBDQ, Inflammatory Bowel Disease Questionnaire; LS, least squares; mBOCF, modified baseline observation carried forward; mITT, modified intent-to-treat; MMS, modified Mayo score; NRI, non-responder imputation; RB, rectal bleeding; SE, standard error; SF, stool frequency.
Baseline was defined as the last nonmissing assessment recorded on or prior to the date of the first study drug administration at Week 0 in LUCENT-1 induction study.
*Within-treatment change from baseline p<0.001 calculated using ANCOVA.
aClinical Responders: Patients who achieved ≥2 points and ≥30% decrease from baseline in MMS and a decrease of ≥1 point in the RB subscore from baseline or an RB score of 0 or 1.
bClinical Remitters: Patients who achieved SF subscore = 0 or 1 with ≥1 point decrease from baseline; RB = 0; ES = 0 or 1.
cBiologic failed: Inadequate response, loss of response, or intolerant to a biologic therapy or Janus kinase inhibitors for UC.
dNot biologic failed: Failed conventional treatments (i.e., immunomodulators/corticosteroids); may include some participants who were exposed to but did not fail biologic treatment.
ANCOVA, analysis of covariance; ES, endoscopic subscore; IBDQ, Inflammatory Bowel Disease Questionnaire; LS, least squares; mBOCF, modified baseline observation carried forward; mITT, modified intent-to-treat; MMS, modified Mayo score; NRI, non-responder imputation; RB, rectal bleeding; SE, standard error; SF, stool frequency.
Disclosures:
Bruce Sands: AbbVie – Consultant. Abivax – Consultant, Speaker’s fees. Adiso Therapeutics – Consultant. Alimentiv – Consultant. Amgen – Consultant. Arena pharmaceuticals – Consultant. Artizan Biosciences – Consultant. Artugen Therapeutics – Consultant. AstraZeneca – Consultant. Bacainn Therapeutics – Consultant. Biora Therapeutics – Consultant. Boehringer Ingelheim – Consultant. Boston Pharmaceuticals – Consultant. Bristol Myers Squibb – Consultant, Grant/Research Support, speaking fees and other support. Calibr – Consultant. Celltrion – Consultant. ClostraBio – Consultant. Connect Biopharm – Consultant. Cytoki Pharma – Consultant. Eli Lilly – Consultant, speaking fees and other support. Enthera – Consultant. Evommune – Consultant. Ferring – Consultant. Fresenius Kabi – Consultant. Galapagos – Consultant. Genentech – Consultant. Gilead Sciences – Consultant. GlaxoSmithKline – Consultant. Gossamer Bio – Consultant. HMP Acquisition – Consultant. Imhotex – Consultant. Immunic – Consultant. InDex Pharmaceuticals – Consultant. Innovation Therapeutics – Consultant. Inotrem – Consultant. Ironwood Pharmaceuticals – Consultant. Janssen – Grant/Research Support, consulting and speaking fees and other support. Johnson & Johnson – Consultant. Kaleido Biosciences – Consultant. Kallyope – Consultant. Merck – Consultant. MiroBio – Consultant. Morphic Therapeutics – Consultant. MRM Health – Consultant. OSE Immunotherapeutics – Consultant. Pfizer Inc – Consultant, Grant/Research Support, speaking fees and other support. Progenity – Consultant. Prometheus Biosciences – Consultant. Prometheus Laboratories – Consultant. Protagonist Therapeutics – Consultant. Q32 Bio – Consultant. RedHill Biopharma – Consultant. Sun Pharma – Consultant. Surrozen – Consultant. Synlogic Operating Company – Consultant. Takeda – Grant/Research Support, consulting and speaking fees and other support. Target RWE – Consultant. Theravance Biopharma – Consultant, Grant/Research Support. TLL Pharmaceutical – Consultant. USWM Enterprises – Consultant. Ventyx Biosciences – Consultant, personal fees and stock options for consulting. Viela Bio – Consultant.
Brian Feagan: AbbVie – Advisory Committee/Board Member, Consultant, Speakers Bureau. AbolerIS – Consultant. AgomAB Therapeutics – Consultant. Allianthera – Consultant. Amgen – Advisory Committee/Board Member, Consultant. AnaptysBio – Consultant. Applied Molecular Transport Inc. – Consultant. Arena Pharma – Consultant. Avir – Consultant. Azora Therapeutics – Consultant. Baxter – Consultant. BioJamp – Consultant. Biora Therapeutics – Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant. Boston Pharma – Consultant. Bristol Myers Squibb – Consultant. Celgene/BMS – Advisory Committee/Board Member, Consultant. Connect BioPharma – Consultant. Cytoki – Consultant. Disc Medicine – Consultant. Duality – Consultant. EcoR1 – Advisory Committee/Board Member, Consultant. Eli Lilly – Consultant. Equillium – Consultant. Ermium – Consultant. Everest Clinical Research Corp. – Consultant. Ferring Pharmaceuticals – Consultant. First Wave – Consultant. Galapagos – Consultant. Galen Atlantica – Consultant. Genentech/Roche – Advisory Committee/Board Member, Consultant. Gilead – Consultant. GlaxoSmithKline – Advisory Committee/Board Member, Consultant. Glenmark – Consultant. Gossamer Pharma – Consultant, stock shareholder. Hoffmann-LaRoche – Consultant. Hot Spot Therapeutics – Consultant. Imhotex – Consultant. ImmunExt – Consultant. Immunic Therapeutics – Consultant. Index Pharma – Advisory Committee/Board Member, Consultant. Intact Therapeutics – Consultant. JAKAcademy – Consultant. Janssen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Japan Tobacco Inc. – Consultant. Kaleido Biosciences – Consultant. L.E.K. Consulting – Consultant. Landos Biopharma – Consultant. Leadiant – Consultant. LifeSci Capital – Consultant. Lument AB – Consultant. Millennium – Consultant. MiroBio – Consultant. Morphic Therapeutics – Advisory Committee/Board Member, Consultant. Mylan – Consultant. Novartis – Advisory Committee/Board Member. OM Pharma – Consultant. Origo BioPharma – Advisory Committee/Board Member, Consultant. Orphagen – Consultant. Otsuka – Consultant. Pandion Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant. Play to Know AG – Consultant. Progenity – Advisory Committee/Board Member, Consultant. Prometheus Therapeutics and Diagnostics – Advisory Committee/Board Member, Consultant. Protagonist – Consultant. PTM Therapeutics – Consultant. Q32 Bio – Consultant. Rebiotix – Consultant. RedHill Biopharma – Consultant. Redx – Consultant. Roche – Consultant. Sandoz – Consultant. Sanofi – Consultant. Seres Therapeutics – Consultant. Silverback Therapeutics – Consultant. Surrozen Inc. – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau. Teva – Advisory Committee/Board Member, Consultant. Thelium – Consultant. Theravance – Consultant. Tigenix – Consultant. Tillotts Pharma – Advisory Committee/Board Member, Consultant. UCB Pharma – Consultant. VHSquared Ltd. – Consultant. Viatris – Consultant. Western University, Alimentiv Inc – Employee. Ysios – Consultant. Ysopia – Consultant. Zealand Pharma – Consultant.
Alessandro Armuzzi: AbbVie – consulting/advisory board fees, speaker’s fees. Allergan – consulting/advisory board fees. Amgen – consulting/advisory board fees, speaker’s fees. Arena – consulting/advisory board fees, speaker’s fees. Biogen – Grant/Research Support, consulting/advisory board fees, speaker’s fees. Boehringer Ingelheim – consulting/advisory board fees. Bristol Myers Squibb – consulting/advisory board fees, speaker’s fees. Celgene – consulting/advisory board fees. Celltrion – consulting/advisory board fees. Eli Lilly – consulting/advisory board fees, speaker’s fees. Ferring – consulting/advisory board fees, speaker’s fees. Galapagos – consulting/advisory board fees, speaker’s fees. Gilead – consulting/advisory board fees, speaker’s fees. Janssen – consulting/advisory board fees, speaker’s fees. MSD – Grant/Research Support, consulting/advisory board fees, speaker’s fees. Mylan – consulting/advisory board fees. Nestlè – consulting/advisory board fees. Novartis – speaker’s fees. Pfizer – Grant/Research Support, consulting/advisory board fees, speaker’s fees. Protagonist Therapeutics – consulting/advisory board fees. Roche – consulting/advisory board fees, speaker’s fees. Samsung Bioepis – consulting/advisory board fees, speaker’s fees. Sandoz – consulting/advisory board fees, speaker’s fees. Takeda – Grant/Research Support, consulting/advisory board fees, speaker’s fees. Tigenix – Speaker’s fees.
Kim McGinnis: Eli Lilly and Company – Employee, Stockholder.
Keisa Lynch: Eli Lilly – Consulting/advisory board fees, Speakers Bureau. Gilead – Grant/Research Support, consulting/advisory board fees, Speakers Bureau. Janssen – consulting/advisory board fees. Pfizer – consulting/advisory board fees.
Theresa Hunter Gibble: Eli Lilly and Company – Employee, stockholder.
Jordan Johns: Eli Lilly and Company – Employee, stockholder.
Corey Siegel: Abbvie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. BMS – Advisory Committee/Board Member, Consultant. Eli Lilly – Advisory Committee/Board Member, Consultant. Fresnius – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Consultant/advisory board, speaker for CME activities. Napo Pharmaceuticals – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support, speaker for CME activities. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau.
Vipul Jairath: AbbVie – Advisory Committee/Board Member, consulting/advisory board fees, speaker’s fees. Alimentiv Inc – consulting/advisory board fees. Arena pharmaceuticals – consulting/advisory board fees. Asahi Kasei Pharma – consulting/advisory board fees. Asieris – consulting/advisory board fees. Astra Zeneca – consulting/advisory board fees. Bristol Myers Squibb – consulting/advisory board fees, speaker’s fees. Celltrion – consulting/advisory board fees. Eli Lilly and Company – consulting/advisory board fees. Ferring – consulting/advisory board fees, speaker’s fees. Flagship Pioneering – consulting/advisory board fees. Fresenius Kabi – consulting/advisory board fees, speaker’s fees. Galapagos – consulting/advisory board fees, speaker’s fees. Genentech – consulting/advisory board fees. Gilead – consulting/advisory board fees. GlaxoSmithKline – consulting/advisory board fees. Janssen – consulting/advisory board fees, speaker’s fees. Merck – consulting/advisory board fees. Metacrine – consulting/advisory board fees. Mylan – consulting/advisory board fees. Pandion – consulting/advisory board fees. Pendopharm – consulting/advisory board fees. Pfizer – consulting/advisory board fees, speaker’s fees. Prometheus – consulting/advisory board fees. Protagonist – consulting/advisory board fees. Reistone Biopharma – consulting/advisory board fees. Roche – consulting/advisory board fees. Sandoz – consulting/advisory board fees. Second Genome – consulting/advisory board fees. Shire – speaker’s fees. Sorriso pharmaceuticals – consulting/advisory board fees. Takeda – consulting/advisory board fees, speaker’s fees. Teva – consulting/advisory board fees. Topivert – consulting/advisory board fees. Ventyx – consulting/advisory board fees. Vividion – consulting/advisory board fees.
Bruce E. Sands, MD, MS, FACG1, Brian G. Feagan, MD2, Alessandro Armuzzi, MD, PhD3, Kim McGinnis, CPNP4, Keisa Lynch, DNP, APRN, FNP5, Theresa Hunter Gibble, PhD, MPH4, Jordan Johns, PhD4, Corey A. Siegel, MD, MS6, Vipul Jairath, MBChB, DPhil2. P2205 - Sustained Improvement in Inflammatory Bowel Disease Questionnaire Outcomes in Moderately to Severely Active Ulcerative Colitis with Continued Mirikizumab Treatment in Phase 3 LUCENT-3 Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
