Monday Poster Session
Category: IBD
P2223 - Risk Factors for Late Postoperative Recurrence of Crohn’s Disease: A Multicenter Retrospective Cohort Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Salam Bachour, MD, MS
Brigham and Women's Hospital, Harvard Medical School
Boston, MA
Presenting Author(s)
Salam Bachour, MD, MS1, Hareem Syed, MD2, Adel Hajj Ali, MD2, Ravi S. Shah, MD2, Abel Joseph, MD2, Terry Li, MD3, Jessica H. Hu, BS4, Vall Vinaithirthan, MD5, Shravya Pothula, MD6, Jeffrey D. Kovach, BS, MS2, Stefan Holubar, MD2, Miguel Regueiro, MD7, Edward Barnes, MD, MPH, FACG8, Jordan Axelrad, MD, MPH9, Ben Cohen, MD, MAS2, Benjamin Click, MD10
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2Cleveland Clinic, Cleveland, OH; 3NYU Langone, New York, NY; 4UNC School of Medicine, Chapel Hill, NC; 5University of Colorado, South Burlington, VT; 6University of Colorado, Aurora, CO; 7Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH; 8University of North Carolina at Chapel Hill, Chapel Hill, NC; 9NYU Grossman School of Medicine, New York, NY; 10University of Colorado, Denver, CO
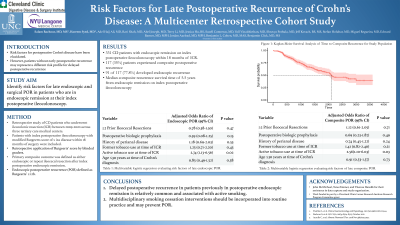
Introduction: Risk factors for delayed postoperative recurrence (POR) of Crohn’s disease (CD) have not been fully elucidated. This study aimed to identify risk factors for late endoscopic and surgical POR in patients who are in endoscopic remission at their index postoperative ileocolonoscopy.
Methods: Retrospective study of CD patients who underwent ileocolonic resection (ICR) between 2009-2020 across three tertiary care medical centers. Patients with index postoperative ileocolonoscopy with modified Rutgeerts score of ≤ i2a disease within 18 months of surgery were included. Primary composite outcome was defined as either endoscopic (Rutgeerts score ≥ i2b) or repeat ICR after index endoscopic remission.
Results: 331 adult CD patients with endoscopic remission on index postoperative ileocolonoscopy within 18 months of ICR. Of these patients, 117 (35%) experienced total composite POR (77.8% endoscopic). On univariate analysis assessing impact of active smoking at time of ICR, age at CD diagnosis, gender, prior history of ICR, history of perianal disease, and postoperative biologic prophylaxis, no variables were associated with composite POR. On multivariable logistic regression, active smoking at time of ICR was associated with a 2.5 times increased risk of composite POR (aOR 2.55 [1.10-6.03]; p=0.03) compared to never smokers. On sensitivity analysis evaluating impact on endoscopic POR, active smoking remained associated with a significantly elevated risk for endoscopic POR compared to non-smokers (aOR 2.73 [1.13-6.56]; p=0.02). In patients who had endoscopic remission on index colonoscopy, the use of postoperative biologic prophylaxis did not offer increased protection against late composite and endoscopic POR (p=0.49; p=0.15).
Discussion: Delayed postoperative recurrence in patients previously in postoperative endoscopic remission is relatively common and associated with active smoking. Multidisciplinary smoking cessation interventions should be incorporated into routine practice and may prevent POR.
Disclosures:
Salam Bachour, MD, MS1, Hareem Syed, MD2, Adel Hajj Ali, MD2, Ravi S. Shah, MD2, Abel Joseph, MD2, Terry Li, MD3, Jessica H. Hu, BS4, Vall Vinaithirthan, MD5, Shravya Pothula, MD6, Jeffrey D. Kovach, BS, MS2, Stefan Holubar, MD2, Miguel Regueiro, MD7, Edward Barnes, MD, MPH, FACG8, Jordan Axelrad, MD, MPH9, Ben Cohen, MD, MAS2, Benjamin Click, MD10. P2223 - Risk Factors for Late Postoperative Recurrence of Crohn’s Disease: A Multicenter Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2Cleveland Clinic, Cleveland, OH; 3NYU Langone, New York, NY; 4UNC School of Medicine, Chapel Hill, NC; 5University of Colorado, South Burlington, VT; 6University of Colorado, Aurora, CO; 7Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH; 8University of North Carolina at Chapel Hill, Chapel Hill, NC; 9NYU Grossman School of Medicine, New York, NY; 10University of Colorado, Denver, CO
Introduction: Risk factors for delayed postoperative recurrence (POR) of Crohn’s disease (CD) have not been fully elucidated. This study aimed to identify risk factors for late endoscopic and surgical POR in patients who are in endoscopic remission at their index postoperative ileocolonoscopy.
Methods: Retrospective study of CD patients who underwent ileocolonic resection (ICR) between 2009-2020 across three tertiary care medical centers. Patients with index postoperative ileocolonoscopy with modified Rutgeerts score of ≤ i2a disease within 18 months of surgery were included. Primary composite outcome was defined as either endoscopic (Rutgeerts score ≥ i2b) or repeat ICR after index endoscopic remission.
Results: 331 adult CD patients with endoscopic remission on index postoperative ileocolonoscopy within 18 months of ICR. Of these patients, 117 (35%) experienced total composite POR (77.8% endoscopic). On univariate analysis assessing impact of active smoking at time of ICR, age at CD diagnosis, gender, prior history of ICR, history of perianal disease, and postoperative biologic prophylaxis, no variables were associated with composite POR. On multivariable logistic regression, active smoking at time of ICR was associated with a 2.5 times increased risk of composite POR (aOR 2.55 [1.10-6.03]; p=0.03) compared to never smokers. On sensitivity analysis evaluating impact on endoscopic POR, active smoking remained associated with a significantly elevated risk for endoscopic POR compared to non-smokers (aOR 2.73 [1.13-6.56]; p=0.02). In patients who had endoscopic remission on index colonoscopy, the use of postoperative biologic prophylaxis did not offer increased protection against late composite and endoscopic POR (p=0.49; p=0.15).
Discussion: Delayed postoperative recurrence in patients previously in postoperative endoscopic remission is relatively common and associated with active smoking. Multidisciplinary smoking cessation interventions should be incorporated into routine practice and may prevent POR.
Disclosures:
Salam Bachour indicated no relevant financial relationships.
Hareem Syed indicated no relevant financial relationships.
Adel Hajj Ali indicated no relevant financial relationships.
Ravi Shah indicated no relevant financial relationships.
Abel Joseph indicated no relevant financial relationships.
Terry Li indicated no relevant financial relationships.
Jessica Hu indicated no relevant financial relationships.
Vall Vinaithirthan indicated no relevant financial relationships.
Shravya Pothula indicated no relevant financial relationships.
Jeffrey Kovach indicated no relevant financial relationships.
Stefan Holubar: Guidepoint – Consultant. Takeda – Consultant.
Miguel Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Alfasigma – Advisory Committee/Board Member, Consultant. Allergan – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Celgene – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Eli Lilly – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Gilead Sciences – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Janssen – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Miraca Labs – Advisory Committee/Board Member, Consultant. Pfizer Inc – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Prometheus – Advisory Committee/Board Member, Consultant. Salix – Advisory Committee/Board Member, Consultant. Seres – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Target RWE – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Wolters Kluwer Health – Royalties.
Edward Barnes: AbbVie, Inc. – Consultant. Bristol-Meyers Squibb – Consultant. Eli Lilly – Consultant. Target RWE – Consultant.
Jordan Axelrad: AbbVie – received consulting fees. Adiso – received consulting fees. BioFire Diagnostics – Consultant, Grant/Research Support. Bristol Myers Squibb – received consulting fees. Fresenius Kabi – received consulting fees. Janssen – received consulting fees. Pfizer – received consulting fees.
Ben Cohen indicated no relevant financial relationships.
Benjamin Click: AbbVie – Consultant. Bristol Meyers Squibb – Consultant. Janssen – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant. Prometheus – Consultant. Takeda – Advisory Committee/Board Member.
Salam Bachour, MD, MS1, Hareem Syed, MD2, Adel Hajj Ali, MD2, Ravi S. Shah, MD2, Abel Joseph, MD2, Terry Li, MD3, Jessica H. Hu, BS4, Vall Vinaithirthan, MD5, Shravya Pothula, MD6, Jeffrey D. Kovach, BS, MS2, Stefan Holubar, MD2, Miguel Regueiro, MD7, Edward Barnes, MD, MPH, FACG8, Jordan Axelrad, MD, MPH9, Ben Cohen, MD, MAS2, Benjamin Click, MD10. P2223 - Risk Factors for Late Postoperative Recurrence of Crohn’s Disease: A Multicenter Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
