Monday Poster Session
Category: IBD
P2225 - The Impact of Intravenous Corticosteroid Therapy in Hospitalized Patients With Inflammatory Bowel Disease with Clostridioides difficile Infection
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Ellen J. Spartz, MD
UCLA
Los Angeles, CA
Presenting Author(s)
Ellen J. Spartz, MD, Andrew Roney, BA, Lauren DeDecker, MD, Shaya Noorian, MD, Kush Fansiwala, MD, Christopher Soriano, MD, Jamie Yang, MD, Shahrad Hakimian, MD, Jenny Sauk, MD, Berkeley Limketkai, MD, PhD
UCLA, Los Angeles, CA
Introduction: Intravenous (IV) corticosteroids are common treatments for patients with inflammatory bowel disease (IBD) who are hospitalized for flares. As IBD patients have an increased risk for developing Clostridioides difficile infections (CDI), and the clinical presentations of an IBD flare and CDI have substantial overlap, the risk-benefit balance for empiric use of IV corticosteroids in these scenarios is unclear. Our study investigates the impact of IV corticosteroid use on outcomes in IBD patients hospitalized for symptoms consistent with a flare and found to have CDI.
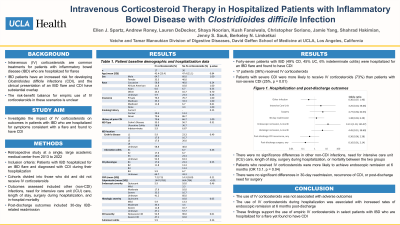
Methods: This retrospective study included patients hospitalized for an IBD flare and diagnosed with CDI during their hospitalization at a single, large academic medical center from 2013 to 2022. Cohorts were divided into those who did and did not receive IV corticosteroids. Outcomes assessed included other infections, need for intensive care unit (ICU) care, length of stay, surgery during hospitalization, and in-hospital mortality. Post-discharge outcomes included 30-day IBD-related readmission, recurrence of CDI, need for IBD-related surgery, and 6-month endoscopic and histologic remission. Multivariable logistic regression was used to evaluate clinical outcomes, adjusted for potential confounders.
Results: Forty-seven patients with IBD (49% Crohn’s disease, 45% ulcerative colitis, 6% indeterminate colitis) were hospitalized for an IBD flare and found to have CDI; 17 patients (36%) received IV corticosteroids (Table 1). Patients with severe CDI were more likely to receive IV corticosteroids (73%) than patients with non-severe CDI (25%, p=0.01). There was no significant difference in other infections, need for ICU care, length of stay, surgery during hospitalization, or mortality between the two groups. Patients who received IV corticosteroids were more likely to achieve endoscopic remission at 6 months (OR 13.1, p=0.04). There were no significant differences in 30-day readmission, recurrence of CDI, or post-discharge need for surgery (Figure 1).
Discussion: In hospitalized patients with IBD, use of IV corticosteroids was more frequently observed in patients with severe CDI. The use of IV corticosteroids was not associated with worse outcomes during hospitalization, although it was associated with increased rates of endoscopic remission at 6 months post-discharge. These findings support the empiric use of IV corticosteroids in select patients with IBD who are hospitalized for a flare yet found to have CDI.

Disclosures:
Ellen J. Spartz, MD, Andrew Roney, BA, Lauren DeDecker, MD, Shaya Noorian, MD, Kush Fansiwala, MD, Christopher Soriano, MD, Jamie Yang, MD, Shahrad Hakimian, MD, Jenny Sauk, MD, Berkeley Limketkai, MD, PhD. P2225 - The Impact of Intravenous Corticosteroid Therapy in Hospitalized Patients With Inflammatory Bowel Disease with Clostridioides difficile Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
UCLA, Los Angeles, CA
Introduction: Intravenous (IV) corticosteroids are common treatments for patients with inflammatory bowel disease (IBD) who are hospitalized for flares. As IBD patients have an increased risk for developing Clostridioides difficile infections (CDI), and the clinical presentations of an IBD flare and CDI have substantial overlap, the risk-benefit balance for empiric use of IV corticosteroids in these scenarios is unclear. Our study investigates the impact of IV corticosteroid use on outcomes in IBD patients hospitalized for symptoms consistent with a flare and found to have CDI.
Methods: This retrospective study included patients hospitalized for an IBD flare and diagnosed with CDI during their hospitalization at a single, large academic medical center from 2013 to 2022. Cohorts were divided into those who did and did not receive IV corticosteroids. Outcomes assessed included other infections, need for intensive care unit (ICU) care, length of stay, surgery during hospitalization, and in-hospital mortality. Post-discharge outcomes included 30-day IBD-related readmission, recurrence of CDI, need for IBD-related surgery, and 6-month endoscopic and histologic remission. Multivariable logistic regression was used to evaluate clinical outcomes, adjusted for potential confounders.
Results: Forty-seven patients with IBD (49% Crohn’s disease, 45% ulcerative colitis, 6% indeterminate colitis) were hospitalized for an IBD flare and found to have CDI; 17 patients (36%) received IV corticosteroids (Table 1). Patients with severe CDI were more likely to receive IV corticosteroids (73%) than patients with non-severe CDI (25%, p=0.01). There was no significant difference in other infections, need for ICU care, length of stay, surgery during hospitalization, or mortality between the two groups. Patients who received IV corticosteroids were more likely to achieve endoscopic remission at 6 months (OR 13.1, p=0.04). There were no significant differences in 30-day readmission, recurrence of CDI, or post-discharge need for surgery (Figure 1).
Discussion: In hospitalized patients with IBD, use of IV corticosteroids was more frequently observed in patients with severe CDI. The use of IV corticosteroids was not associated with worse outcomes during hospitalization, although it was associated with increased rates of endoscopic remission at 6 months post-discharge. These findings support the empiric use of IV corticosteroids in select patients with IBD who are hospitalized for a flare yet found to have CDI.

Figure: Figure 1. Hospitalization and post-discharge outcomes
Disclosures:
Ellen Spartz indicated no relevant financial relationships.
Andrew Roney indicated no relevant financial relationships.
Lauren DeDecker indicated no relevant financial relationships.
Shaya Noorian indicated no relevant financial relationships.
Kush Fansiwala indicated no relevant financial relationships.
Christopher Soriano indicated no relevant financial relationships.
Jamie Yang indicated no relevant financial relationships.
Shahrad Hakimian indicated no relevant financial relationships.
Jenny Sauk indicated no relevant financial relationships.
Berkeley Limketkai: Azora Therapeutics – Consultant, Stock-privately held company.
Ellen J. Spartz, MD, Andrew Roney, BA, Lauren DeDecker, MD, Shaya Noorian, MD, Kush Fansiwala, MD, Christopher Soriano, MD, Jamie Yang, MD, Shahrad Hakimian, MD, Jenny Sauk, MD, Berkeley Limketkai, MD, PhD. P2225 - The Impact of Intravenous Corticosteroid Therapy in Hospitalized Patients With Inflammatory Bowel Disease with Clostridioides difficile Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
