Monday Poster Session
Category: IBD
P2229 - Double Trouble: A Rare Case of Concurrent Severe H. pylori Infection and Ulcerative Colitis as Initial Presentation
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Arturo Suplee Rivera, MD
University of Texas
Edinburg, Texas
Presenting Author(s)
Arturo Suplee Rivera, MD1, Prateek S. Harne, MBBS, MD2, Ans Albustamy, MD3, Henry Herrera, MD4, Asif Zamir, MD, FACG5
1University of Texas, Edinburg, TX; 2University of Texas, Houston, TX; 3DHR, McAllen, TX; 4University of Texas at DHR, Edinburg, TX; 5DHR Health Gastroenterology, Edinburg, TX
Introduction: Helicobacter pylori (H. pylori) is a gram-negative bacterium that causes chronic gastritis and may play important role in peptic ulcer, gastric carcinoma and lymphoma. Ulcerative colitis (UC) is an inflammatory bowel disease (IBD) of the colon with unidentified cause. Genetic and environmental elements, in particular the gut bacteria appear to play a role in its pathogenesis. There are controversial reports about the inverse association between presence of H. pylori infection and presence and severity of IBD. We present a case of a patient with initial presentation of UC flare concurrent with severe H. pylori gastritis.
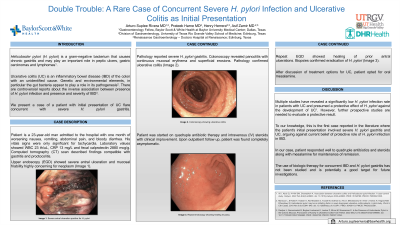
Case Description/Methods: Patient is a 23-year-old man admitted to the hospital with one month of worsening nausea, vomiting, abdominal pain, and bloody diarrhea. His vitals only significant for tachycardia. Laboratory values showed WBC 23 th/uL, CRP 13 mg/L and fecal calprotectin 2880 mcg/g. CT scan described findings compatible with gastritis and proctocolitis. Upper endoscopy (EGD) showed severe antral ulceration and mucosal friability highly concerning for neoplasm. Pathology reported severe H. pylori gastritis. Colonoscopy revealed pancolitis with continuous mucosal erythema and superficial erosions; Pathology confirmed ulcerative colitis. Patient was started on quadruple antibiotic therapy and IV steroids with clinical improvement. Upon outpatient follow up, patient was found completely asymptomatic. Repeat EGD showed healing of prior antral ulcerations. Biopsies confirmed eradication of H. pylori. After discussion of treatment options for UC, patient opted for oral mesalamine.
Discussion: Multiple studies have revealed a significantly low H. pylori infection rate in patients with UC and presumed a protective effect of H. pylori against the development of UC. However, further prospective studies are needed to evaluate a protective result. To our knowledge, this case is the first reported in literature where the patient initial presentation involved severe H. pylori gastritis and UC, arguing against current belief of protective role of H. pylori infection in IBD. In our case, patient responded well to quadruple antibiotics and steroids along with mesalamine for maintenance of remission. The use of biologic therapy for concurrent IBD and H. pylori gastritis has not been studied and is potentially a good target for future investigations.

Disclosures:
Arturo Suplee Rivera, MD1, Prateek S. Harne, MBBS, MD2, Ans Albustamy, MD3, Henry Herrera, MD4, Asif Zamir, MD, FACG5. P2229 - Double Trouble: A Rare Case of Concurrent Severe H. pylori Infection and Ulcerative Colitis as Initial Presentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas, Edinburg, TX; 2University of Texas, Houston, TX; 3DHR, McAllen, TX; 4University of Texas at DHR, Edinburg, TX; 5DHR Health Gastroenterology, Edinburg, TX
Introduction: Helicobacter pylori (H. pylori) is a gram-negative bacterium that causes chronic gastritis and may play important role in peptic ulcer, gastric carcinoma and lymphoma. Ulcerative colitis (UC) is an inflammatory bowel disease (IBD) of the colon with unidentified cause. Genetic and environmental elements, in particular the gut bacteria appear to play a role in its pathogenesis. There are controversial reports about the inverse association between presence of H. pylori infection and presence and severity of IBD. We present a case of a patient with initial presentation of UC flare concurrent with severe H. pylori gastritis.
Case Description/Methods: Patient is a 23-year-old man admitted to the hospital with one month of worsening nausea, vomiting, abdominal pain, and bloody diarrhea. His vitals only significant for tachycardia. Laboratory values showed WBC 23 th/uL, CRP 13 mg/L and fecal calprotectin 2880 mcg/g. CT scan described findings compatible with gastritis and proctocolitis. Upper endoscopy (EGD) showed severe antral ulceration and mucosal friability highly concerning for neoplasm. Pathology reported severe H. pylori gastritis. Colonoscopy revealed pancolitis with continuous mucosal erythema and superficial erosions; Pathology confirmed ulcerative colitis. Patient was started on quadruple antibiotic therapy and IV steroids with clinical improvement. Upon outpatient follow up, patient was found completely asymptomatic. Repeat EGD showed healing of prior antral ulcerations. Biopsies confirmed eradication of H. pylori. After discussion of treatment options for UC, patient opted for oral mesalamine.
Discussion: Multiple studies have revealed a significantly low H. pylori infection rate in patients with UC and presumed a protective effect of H. pylori against the development of UC. However, further prospective studies are needed to evaluate a protective result. To our knowledge, this case is the first reported in literature where the patient initial presentation involved severe H. pylori gastritis and UC, arguing against current belief of protective role of H. pylori infection in IBD. In our case, patient responded well to quadruple antibiotics and steroids along with mesalamine for maintenance of remission. The use of biologic therapy for concurrent IBD and H. pylori gastritis has not been studied and is potentially a good target for future investigations.

Figure: Image 1: a) Colonoscopy showing ulcerative colitis. b) Severe antral ulceration positive for H pylori. c) Repeat endoscopy showing healing mucosa.
Disclosures:
Arturo Suplee Rivera indicated no relevant financial relationships.
Prateek Harne indicated no relevant financial relationships.
Ans Albustamy indicated no relevant financial relationships.
Henry Herrera indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Arturo Suplee Rivera, MD1, Prateek S. Harne, MBBS, MD2, Ans Albustamy, MD3, Henry Herrera, MD4, Asif Zamir, MD, FACG5. P2229 - Double Trouble: A Rare Case of Concurrent Severe H. pylori Infection and Ulcerative Colitis as Initial Presentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

