Monday Poster Session
Category: Interventional Endoscopy
P2281 - Cystic Duct Stenting vs Other Treatment Modalities for Management of Acute Cholecystitis in Patients With Decompensated Cirrhosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Muhammad Salman Faisal, MD
Henry Ford Health System
Detroit, MI
Presenting Author(s)
Award: Presidential Poster Award
Muhammad Salman Faisal, MD1, Taha Ashraf, MD1, Kevin Harris, MD2, Muhammad Zarrar Khan, MD2, Ammad Chaudhary, MD2, Andrew Watson, MD2, Duyen Dang, MD2, Robert Pompa, MD2, Mazen Elatrache, MD2, Cyrus Piraka, MD2, Sumit Singla, MD2, Tobias Zuchelli, MD2
1Henry Ford Health System, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
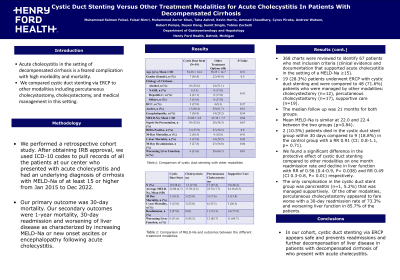
Introduction: Acute cholecystitis in the setting of decompensated cirrhosis is a feared complication with high morbidity and mortality. We compared outcomes of cystic duct stenting via ERCP to other modalities including percutaneous cholecystostomy, cholecystectomy, and medical management in this setting.
Methods: We performed a retrospective cohort study. After obtaining IRB approval, we used ICD-10 codes to identify patients who presented with acute cholecystitis and had an underlying diagnosis of cirrhosis with MELD-Na of at least 15 or higher from Jan 2015 to Dec 2022 at our center. Primary outcome was 30-day mortality. Our secondary outcomes were 1-year mortality, 30-day readmission and worsening of liver disease as characterized by increasing MELD-Na or new onset ascites or encephalopathy following acute cholecystitis.
Results: 368 charts were reviewed to identify 67 patients who met inclusion criteria (clinical evidence and documentation that supported acute cholecystitis in the setting of a MELD-Na ≥15). 19 (28.3%) patients underwent ERCP with cystic duct stenting and were compared to 48 (71.6%) patients who were managed by other modalities: cholecystectomy (n=12), percutaneous cholecystostomy (n=17), supportive care (n=19). The median follow up was 21 months for both groups. There was no major difference in demographics, etiology of cirrhosis, hepatocellular cancer(p=0.37) presence of ascites (p=0.67) and encephalopathy (p=0.54) between the two groups. Mean MELD-Na is similar at 22.0 and 22.4 between the two groups (p=0.84). 2 (10.5%) patients died in the cystic duct stent group due to complications of cirrhosis within 30 days compared to 9 (18.8%) in the control group with a RR 0.91 (CI: 0.8-1.1, p= 0.71). We found a significant difference in the protective effect of cystic duct stenting compared to other modalities on one month readmission rate and decline in liver function with RR of 0.56 (0.4-0.9, P= 0.038) and RR 0.49 (CI 0.3-0.8, P= 0.01) respectively. The only complication in the cystic duct stent group was pancreatitis (n=1, 5.2%) that was managed supportively. Percutaneous cholecystostomy had the highest rates of 30-day readmission (73.3%) and worsening liver function (85.7%).
Discussion: In our cohort, cystic duct stenting via ERCP appears safe and prevents readmissions and further decompensation of liver disease in patients with decompensated cirrhosis who present with acute cholecystitis.
Disclosures:
Muhammad Salman Faisal, MD1, Taha Ashraf, MD1, Kevin Harris, MD2, Muhammad Zarrar Khan, MD2, Ammad Chaudhary, MD2, Andrew Watson, MD2, Duyen Dang, MD2, Robert Pompa, MD2, Mazen Elatrache, MD2, Cyrus Piraka, MD2, Sumit Singla, MD2, Tobias Zuchelli, MD2. P2281 - Cystic Duct Stenting vs Other Treatment Modalities for Management of Acute Cholecystitis in Patients With Decompensated Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Muhammad Salman Faisal, MD1, Taha Ashraf, MD1, Kevin Harris, MD2, Muhammad Zarrar Khan, MD2, Ammad Chaudhary, MD2, Andrew Watson, MD2, Duyen Dang, MD2, Robert Pompa, MD2, Mazen Elatrache, MD2, Cyrus Piraka, MD2, Sumit Singla, MD2, Tobias Zuchelli, MD2
1Henry Ford Health System, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Acute cholecystitis in the setting of decompensated cirrhosis is a feared complication with high morbidity and mortality. We compared outcomes of cystic duct stenting via ERCP to other modalities including percutaneous cholecystostomy, cholecystectomy, and medical management in this setting.
Methods: We performed a retrospective cohort study. After obtaining IRB approval, we used ICD-10 codes to identify patients who presented with acute cholecystitis and had an underlying diagnosis of cirrhosis with MELD-Na of at least 15 or higher from Jan 2015 to Dec 2022 at our center. Primary outcome was 30-day mortality. Our secondary outcomes were 1-year mortality, 30-day readmission and worsening of liver disease as characterized by increasing MELD-Na or new onset ascites or encephalopathy following acute cholecystitis.
Results: 368 charts were reviewed to identify 67 patients who met inclusion criteria (clinical evidence and documentation that supported acute cholecystitis in the setting of a MELD-Na ≥15). 19 (28.3%) patients underwent ERCP with cystic duct stenting and were compared to 48 (71.6%) patients who were managed by other modalities: cholecystectomy (n=12), percutaneous cholecystostomy (n=17), supportive care (n=19). The median follow up was 21 months for both groups. There was no major difference in demographics, etiology of cirrhosis, hepatocellular cancer(p=0.37) presence of ascites (p=0.67) and encephalopathy (p=0.54) between the two groups. Mean MELD-Na is similar at 22.0 and 22.4 between the two groups (p=0.84). 2 (10.5%) patients died in the cystic duct stent group due to complications of cirrhosis within 30 days compared to 9 (18.8%) in the control group with a RR 0.91 (CI: 0.8-1.1, p= 0.71). We found a significant difference in the protective effect of cystic duct stenting compared to other modalities on one month readmission rate and decline in liver function with RR of 0.56 (0.4-0.9, P= 0.038) and RR 0.49 (CI 0.3-0.8, P= 0.01) respectively. The only complication in the cystic duct stent group was pancreatitis (n=1, 5.2%) that was managed supportively. Percutaneous cholecystostomy had the highest rates of 30-day readmission (73.3%) and worsening liver function (85.7%).
Discussion: In our cohort, cystic duct stenting via ERCP appears safe and prevents readmissions and further decompensation of liver disease in patients with decompensated cirrhosis who present with acute cholecystitis.
Disclosures:
Muhammad Salman Faisal indicated no relevant financial relationships.
Taha Ashraf indicated no relevant financial relationships.
Kevin Harris indicated no relevant financial relationships.
Muhammad Zarrar Khan indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Andrew Watson indicated no relevant financial relationships.
Duyen Dang indicated no relevant financial relationships.
Robert Pompa indicated no relevant financial relationships.
Mazen Elatrache indicated no relevant financial relationships.
Cyrus Piraka: Boston Scientific – Consultant.
Sumit Singla: Boston Scientific – Consultant.
Tobias Zuchelli: Boston Scientific – Consultant.
Muhammad Salman Faisal, MD1, Taha Ashraf, MD1, Kevin Harris, MD2, Muhammad Zarrar Khan, MD2, Ammad Chaudhary, MD2, Andrew Watson, MD2, Duyen Dang, MD2, Robert Pompa, MD2, Mazen Elatrache, MD2, Cyrus Piraka, MD2, Sumit Singla, MD2, Tobias Zuchelli, MD2. P2281 - Cystic Duct Stenting vs Other Treatment Modalities for Management of Acute Cholecystitis in Patients With Decompensated Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

