Monday Poster Session
Category: Interventional Endoscopy
P2322 - Successful Endoscopic Submucosal Dissection of a Gastroesophageal Junction Adenocarcinoma in a Patient with a Severe Bleeding Diathesis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- AE
Ahmed Eltelbany, MD, MPH
Cleveland Clinic
Albuquerque, NM
Presenting Author(s)
Ahmed Eltelbany, MD, MPH1, Sandra Mazzoni, DO1, John Vargo, MD1, Sudish Murthy, MD2, Siva Raja, MD2, Amit Bhatt, MD1
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH
Introduction: Endoscopic submucosal dissection (ESD) is a challenging yet preferred treatment modality for early-stage gastroesophageal junction (GEJ) tumors. However, the procedure's complexity is significantly amplified in patients presenting with a severe bleeding diathesis such as plasminogen activator inhibitor-1 (PAI-1) deficiency. In this case report, we present a patient with PAI-1 deficiency who underwent successful ESD of a T1a GEJ tumor.
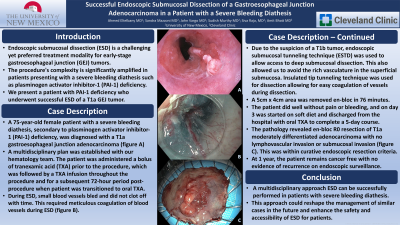
Case Description/Methods: A 75-year-old female patient with a severe bleeding diathesis, secondary to PAI-1 deficiency, was diagnosed with a T1b GEJ adenocarcinoma (fig A), based on endoscopic ultrasound and positron emission tomography/computed tomography (PET/CT) scan findings. The patient underwent an attempted endoscopic ESD at an outside hospital that was aborted due to bleeding and was referred to our institution for esophagectomy. Our surgeons asked us for our second opinion. A multidisciplinary plan was established with our hematology team. The patient was administered a bolus of tranexamic acid (TXA) prior to the procedure, which was followed by a TXA infusion throughout the procedure and for a subsequent 72-hour period post-procedure when patient was transitioned to oral TXA. During ESD, even small blood vessels bled and did not clot off with time. This required meticulous coagulation of blood vessels during ESD (fig B & C). Due to the suspicion of a T1b tumor, endoscopic submucosal tunneling technique (ESTD) was used to allow deep submucosal dissection. This also allowed us to avoid the rich vasculature in the superficial submucosa. Insulated tip tunneling technique was used for dissection allowing for easy coagulation of vessels during dissection. A 5cmx4cm area was removed en-bloc in 76 minutes. The patient was admitted to the hospital for observation after the procedure. The patient did well without pain or bleeding, and on day 3 was started on soft diet and discharged with oral TXA to complete a 5-day course. Pathology revealed en-bloc R0 resection of T1a moderately differentiated adenocarcinoma with no lymphovascular invasion or submucosal invasion (fig D). This was within curative endoscopic resection criteria. At 1 year, the patient remains cancer free with no evidence of recurrence on endoscopic surveillance.
Discussion: This case highlights that with a multidisciplinary approach ESD can be successfully performed in patients with severe bleeding diathesis. This approach could reshape the management of similar cases and enhance the safety of ESD.

Disclosures:
Ahmed Eltelbany, MD, MPH1, Sandra Mazzoni, DO1, John Vargo, MD1, Sudish Murthy, MD2, Siva Raja, MD2, Amit Bhatt, MD1. P2322 - Successful Endoscopic Submucosal Dissection of a Gastroesophageal Junction Adenocarcinoma in a Patient with a Severe Bleeding Diathesis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH
Introduction: Endoscopic submucosal dissection (ESD) is a challenging yet preferred treatment modality for early-stage gastroesophageal junction (GEJ) tumors. However, the procedure's complexity is significantly amplified in patients presenting with a severe bleeding diathesis such as plasminogen activator inhibitor-1 (PAI-1) deficiency. In this case report, we present a patient with PAI-1 deficiency who underwent successful ESD of a T1a GEJ tumor.
Case Description/Methods: A 75-year-old female patient with a severe bleeding diathesis, secondary to PAI-1 deficiency, was diagnosed with a T1b GEJ adenocarcinoma (fig A), based on endoscopic ultrasound and positron emission tomography/computed tomography (PET/CT) scan findings. The patient underwent an attempted endoscopic ESD at an outside hospital that was aborted due to bleeding and was referred to our institution for esophagectomy. Our surgeons asked us for our second opinion. A multidisciplinary plan was established with our hematology team. The patient was administered a bolus of tranexamic acid (TXA) prior to the procedure, which was followed by a TXA infusion throughout the procedure and for a subsequent 72-hour period post-procedure when patient was transitioned to oral TXA. During ESD, even small blood vessels bled and did not clot off with time. This required meticulous coagulation of blood vessels during ESD (fig B & C). Due to the suspicion of a T1b tumor, endoscopic submucosal tunneling technique (ESTD) was used to allow deep submucosal dissection. This also allowed us to avoid the rich vasculature in the superficial submucosa. Insulated tip tunneling technique was used for dissection allowing for easy coagulation of vessels during dissection. A 5cmx4cm area was removed en-bloc in 76 minutes. The patient was admitted to the hospital for observation after the procedure. The patient did well without pain or bleeding, and on day 3 was started on soft diet and discharged with oral TXA to complete a 5-day course. Pathology revealed en-bloc R0 resection of T1a moderately differentiated adenocarcinoma with no lymphovascular invasion or submucosal invasion (fig D). This was within curative endoscopic resection criteria. At 1 year, the patient remains cancer free with no evidence of recurrence on endoscopic surveillance.
Discussion: This case highlights that with a multidisciplinary approach ESD can be successfully performed in patients with severe bleeding diathesis. This approach could reshape the management of similar cases and enhance the safety of ESD.

Figure: Composite Figure (A: T1a Gastroesophageal junction adenocarcinoma, B/C: Endoscopic submucosal dissection of lesion D: En-bloc R0 resection of T1a moderately differentiated adenocarcinoma with no lymphovascular invasion or submucosal invasion)
Disclosures:
Ahmed Eltelbany indicated no relevant financial relationships.
Sandra Mazzoni indicated no relevant financial relationships.
John Vargo indicated no relevant financial relationships.
Sudish Murthy indicated no relevant financial relationships.
Siva Raja indicated no relevant financial relationships.
Amit Bhatt: Boston Scientific – Consultant. Medtronic – Consultant, Intellectual Property/Patents. Steris – Consultant.
Ahmed Eltelbany, MD, MPH1, Sandra Mazzoni, DO1, John Vargo, MD1, Sudish Murthy, MD2, Siva Raja, MD2, Amit Bhatt, MD1. P2322 - Successful Endoscopic Submucosal Dissection of a Gastroesophageal Junction Adenocarcinoma in a Patient with a Severe Bleeding Diathesis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
