Monday Poster Session
Category: Interventional Endoscopy
P2323 - Safety and Efficacy of Biliary Radiofrequency Ablation in Management of Ampullary Lesions
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Muhammad Salman Faisal, MD
Henry Ford Health System
Detroit, MI
Presenting Author(s)
Muhammad Salman Faisal, MD1, Omar Shamaa, MD1, Duyen Dang, MD2, Andrew Watson, MD2, Mazen Elatrache, MD2, Robert Pompa, MD2, Tobias Zuchelli, MD2, Cyrus Piraka, MD2, Sumit Singla, MD2
1Henry Ford Health System, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Ampullary adenoma removal via endoscopic ampullectomy can be challenging especially if it extends into the common bile duct or pancreatic duct. We retrospectively evaluated the safety and clinical success of biliary radiofrequency ablation (RFA) using endoscopically applied probe during ERCP as an adjunct to the management of these lesions.
Case Description/Methods: After approval of local IRB, patients who undergo biliary RFA for ampullary lesions were included in the study from Jan 2018 to May 2023. Individual charts were then reviewed to gather data. Clinical success was defined as no recurrence on follow up endoscopy. We also looked for complications such as bleeding, perforation, pancreatitis, infection, and death. Information was gathered from the date of the procedure involving biliary RFA till the last follow-up.
Four patients underwent biliary RFA for ampullary lesions at our institution. The mean age of our patients was 75.75 ± 7.1 years. Fifty percent were female. Three patients had ampullary adenoma extending into the bile duct as the indication while one patient had pathology consistent with ampullary adenoacarcinoma but was a poor surgical candidate due to underlying cirrhosis. After multidisciplinary discussion, she underwent endoscopic ampullectomy and biliary RFA. She is also getting concomitant chemotherapy with capecitabine and systemic radiation of 50.4 Gy in 28 sessions. We have long term follow up data on two of the patients close to four years with no evidence of recurrence on subsequent follow up ERCP procedures. Biliary RFA was technically successful in all patients. One patient had non severe post procedural bleeding from duodenal ulcer that was managed supportively. No major complications were encountered post procedure for any patient. All patients had prior ERCPs and had plastic biliary stents in place at the time of this procedure. Plastics stents were replaced with covered metal stent in all cases. None of the patients experienced pancreatitis, perforation, infection, significant bleeding, or death following the procedure.
Discussion: Biliary RFA treatment as an adjunct for management ampullary lesions extending into the common bile duct and pancreatic duct appears to be technically feasible and safe with no recurrence in our case series. Further larger scale and multicenter studies are needed to identify patient and disease specific characteristics that will best benefit from this treatment modality.

Disclosures:
Muhammad Salman Faisal, MD1, Omar Shamaa, MD1, Duyen Dang, MD2, Andrew Watson, MD2, Mazen Elatrache, MD2, Robert Pompa, MD2, Tobias Zuchelli, MD2, Cyrus Piraka, MD2, Sumit Singla, MD2. P2323 - Safety and Efficacy of Biliary Radiofrequency Ablation in Management of Ampullary Lesions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Henry Ford Health System, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Ampullary adenoma removal via endoscopic ampullectomy can be challenging especially if it extends into the common bile duct or pancreatic duct. We retrospectively evaluated the safety and clinical success of biliary radiofrequency ablation (RFA) using endoscopically applied probe during ERCP as an adjunct to the management of these lesions.
Case Description/Methods: After approval of local IRB, patients who undergo biliary RFA for ampullary lesions were included in the study from Jan 2018 to May 2023. Individual charts were then reviewed to gather data. Clinical success was defined as no recurrence on follow up endoscopy. We also looked for complications such as bleeding, perforation, pancreatitis, infection, and death. Information was gathered from the date of the procedure involving biliary RFA till the last follow-up.
Four patients underwent biliary RFA for ampullary lesions at our institution. The mean age of our patients was 75.75 ± 7.1 years. Fifty percent were female. Three patients had ampullary adenoma extending into the bile duct as the indication while one patient had pathology consistent with ampullary adenoacarcinoma but was a poor surgical candidate due to underlying cirrhosis. After multidisciplinary discussion, she underwent endoscopic ampullectomy and biliary RFA. She is also getting concomitant chemotherapy with capecitabine and systemic radiation of 50.4 Gy in 28 sessions. We have long term follow up data on two of the patients close to four years with no evidence of recurrence on subsequent follow up ERCP procedures. Biliary RFA was technically successful in all patients. One patient had non severe post procedural bleeding from duodenal ulcer that was managed supportively. No major complications were encountered post procedure for any patient. All patients had prior ERCPs and had plastic biliary stents in place at the time of this procedure. Plastics stents were replaced with covered metal stent in all cases. None of the patients experienced pancreatitis, perforation, infection, significant bleeding, or death following the procedure.
Discussion: Biliary RFA treatment as an adjunct for management ampullary lesions extending into the common bile duct and pancreatic duct appears to be technically feasible and safe with no recurrence in our case series. Further larger scale and multicenter studies are needed to identify patient and disease specific characteristics that will best benefit from this treatment modality.

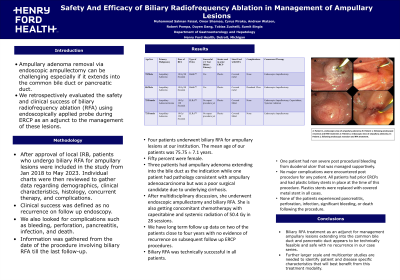
Figure: A: Patient 1, endoscopic view of ampullary adenoma; B: Patient 1, following endoscopic resection and RFA treatment; C: Patient 2, endoscopic view of ampullary adenoma; D: Patient 2, following endoscopic resection and RFA treatment.
Disclosures:
Muhammad Salman Faisal indicated no relevant financial relationships.
Omar Shamaa indicated no relevant financial relationships.
Duyen Dang indicated no relevant financial relationships.
Andrew Watson indicated no relevant financial relationships.
Mazen Elatrache indicated no relevant financial relationships.
Robert Pompa indicated no relevant financial relationships.
Tobias Zuchelli: Boston Scientific – Consultant.
Cyrus Piraka: Boston Scientific – Consultant.
Sumit Singla: Boston Scientific – Consultant.
Muhammad Salman Faisal, MD1, Omar Shamaa, MD1, Duyen Dang, MD2, Andrew Watson, MD2, Mazen Elatrache, MD2, Robert Pompa, MD2, Tobias Zuchelli, MD2, Cyrus Piraka, MD2, Sumit Singla, MD2. P2323 - Safety and Efficacy of Biliary Radiofrequency Ablation in Management of Ampullary Lesions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
