Monday Poster Session
Category: Liver
P2356 - Impact of the COVID-19 Pandemic on Hepatitis B Vaccinations: A Single Large Academic Center Experience
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- EB
Edward Butt, MD, MPH
UTMB
Galveston, TX
Presenting Author(s)
Edward Butt, MD, MPH1, Julia Zhang, MD2, Akshata Moghe, MD, PhD1, Brooke Corning, MD2
1UTMB, Galveston, TX; 2University of Texas Medical Branch, Galveston, TX
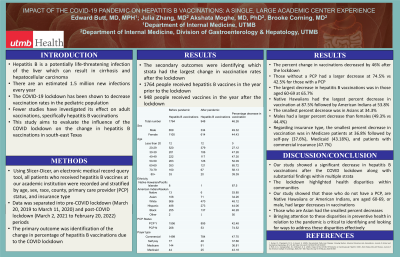
Introduction: Hepatitis B is a potentially life-threatening infection of the liver which can result in cirrhosis and hepatocellular carcinoma. There are an estimated 1.5 million new infections every year. The COVID-19 lockdown has been shown to decrease vaccination rates in the pediatric population. Fewer studies have investigated its effect on adult vaccinations, specifically hepatitis B vaccinations.
Methods: Using Slicer-Dicer, an electronic medical record query tool, all patients who received hepatitis B vaccines were recorded at an academic institution and stratified by age, sex, race, county, primary care provider (PCP) status, and insurance type. Data was separated into pre-COVID lockdown (March 20, 2019 to March 11, 2020) and post-COVID lockdown (March 2, 2021 to February 20, 2022) periods. The primary outcome was identification of the change in percentage of hepatitis B vaccinations due to the COVID lockdown. The secondary outcomes were identifying which strata had the largest change in vaccination rates after the lockdown.
Results: 1764 people received hepatitis B vaccines in the year prior to the lockdown while 948 people received vaccines in the year after the lockdown. The percent change in vaccinations decreased by 46% after the lockdown. Those without a PCP had a larger decrease at 74.5% vs 42.5% for those with a PCP. The largest decrease in hepatitis B vaccines was in those aged 60-69 at 65.7%. Native Hawaiians had the largest percent decrease in vaccination at 87.5% followed by American Indians at 53.8%. The smallest percent decrease was in Asians at 34.3%. Males had a larger percent decrease than females (49.3% vs 44.4%). Regarding insurance type, the smallest percent decrease in vaccination was in Medicare patients at 36.8%, followed by self-pay (37.6%), Medicaid (43.18%), and patients with commercial insurance (47.7%).
Discussion: Our study showed a significant decrease in hepatitis B vaccinations after the COVID lockdown along with substantial findings within multiple strata. The lockdown highlighted health disparities within communities. Our study showed that those who did not have a PCP, are Native Hawaiians or American Indians, are aged 60-69, or male, had larger decreases in vaccinations. Additionally, those with Medicare, and those who are Asian had the smallest percent decreases. Bringing attention to these disparities in preventive health in relation to the pandemic is critical to identifying ways to address these key issues appropriately.
Disclosures:
Edward Butt, MD, MPH1, Julia Zhang, MD2, Akshata Moghe, MD, PhD1, Brooke Corning, MD2. P2356 - Impact of the COVID-19 Pandemic on Hepatitis B Vaccinations: A Single Large Academic Center Experience, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UTMB, Galveston, TX; 2University of Texas Medical Branch, Galveston, TX
Introduction: Hepatitis B is a potentially life-threatening infection of the liver which can result in cirrhosis and hepatocellular carcinoma. There are an estimated 1.5 million new infections every year. The COVID-19 lockdown has been shown to decrease vaccination rates in the pediatric population. Fewer studies have investigated its effect on adult vaccinations, specifically hepatitis B vaccinations.
Methods: Using Slicer-Dicer, an electronic medical record query tool, all patients who received hepatitis B vaccines were recorded at an academic institution and stratified by age, sex, race, county, primary care provider (PCP) status, and insurance type. Data was separated into pre-COVID lockdown (March 20, 2019 to March 11, 2020) and post-COVID lockdown (March 2, 2021 to February 20, 2022) periods. The primary outcome was identification of the change in percentage of hepatitis B vaccinations due to the COVID lockdown. The secondary outcomes were identifying which strata had the largest change in vaccination rates after the lockdown.
Results: 1764 people received hepatitis B vaccines in the year prior to the lockdown while 948 people received vaccines in the year after the lockdown. The percent change in vaccinations decreased by 46% after the lockdown. Those without a PCP had a larger decrease at 74.5% vs 42.5% for those with a PCP. The largest decrease in hepatitis B vaccines was in those aged 60-69 at 65.7%. Native Hawaiians had the largest percent decrease in vaccination at 87.5% followed by American Indians at 53.8%. The smallest percent decrease was in Asians at 34.3%. Males had a larger percent decrease than females (49.3% vs 44.4%). Regarding insurance type, the smallest percent decrease in vaccination was in Medicare patients at 36.8%, followed by self-pay (37.6%), Medicaid (43.18%), and patients with commercial insurance (47.7%).
Discussion: Our study showed a significant decrease in hepatitis B vaccinations after the COVID lockdown along with substantial findings within multiple strata. The lockdown highlighted health disparities within communities. Our study showed that those who did not have a PCP, are Native Hawaiians or American Indians, are aged 60-69, or male, had larger decreases in vaccinations. Additionally, those with Medicare, and those who are Asian had the smallest percent decreases. Bringing attention to these disparities in preventive health in relation to the pandemic is critical to identifying ways to address these key issues appropriately.
Disclosures:
Edward Butt indicated no relevant financial relationships.
Julia Zhang indicated no relevant financial relationships.
Akshata Moghe indicated no relevant financial relationships.
Brooke Corning indicated no relevant financial relationships.
Edward Butt, MD, MPH1, Julia Zhang, MD2, Akshata Moghe, MD, PhD1, Brooke Corning, MD2. P2356 - Impact of the COVID-19 Pandemic on Hepatitis B Vaccinations: A Single Large Academic Center Experience, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
