Monday Poster Session
Category: Liver
P2372 - Bias-Influenced Misdiagnosis of NAFLD in the African American Community
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Astha Saini, DO
Wayne State University School of Medicine / Detroit Medical Center
Detroit, MI
Presenting Author(s)
Astha Saini, DO1, Anirudh R. Damughatla, DO1, Paul H. Naylor, PhD2, Milton G. Mutchnick, MD2
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Wayne State University School of Medicine, Detroit, MI
Introduction: Nonalcoholic fatty liver disease (NAFLD) is becoming the most common chronic liver disease in the United States. Accurate diagnosis is mandatory as advanced fibrosis (NASH) is a predictor of liver-related mortality and requires close monitoring. The African American (AA) population has a known low incidence of NAFLD. We sought to assess if there was a similar trend in our patient (pt) population. During our data analysis, we found that African American individuals were more likely to be misdiagnosed.
Methods: Using ICD-10 codes, we identified pts between 2017 and 2020 who had the diagnosis of NAFLD (K76.0) or NASH (K75.81). We defined NAFLD pts as those with significant steatosis and minimal fibrosis and NASH pts as those with significant steatosis and advanced fibrosis (F2-F4).
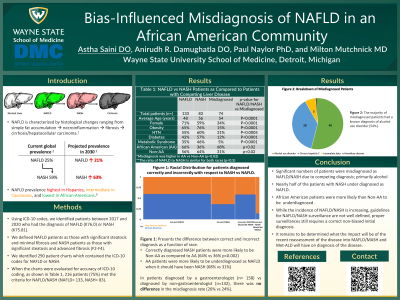
Results: We identified 290 pts charts which contained the ICD-10 codes for NAFLD and NASH. The charts were evaluated for accuracy of ICD-10 coding, 216 pts (75%) met the criteria for NAFLD/NASH and 74 pts had other competing liver disease (Table 1). We divided pts into those diagnosed by a gastroenterologist (GI) (n= 158) vs Non-GI (n=132), there was no difference in the misdiagnosis rate (26% vs 24%). Of the 216 pts who met criteria for either NAFLD or NASH, 39 pts were diagnosed with NAFLD but met the criteria for NASH. These underdiagnosed pts were half the total number of pts with NASH in our pt pool. In contrast, only 7 pts were incorrectly diagnosed with NASH but did not have fibrosis and thus met the criteria for NAFLD (7/46, 15%). When racial disparity was assessed, AA pts were more likely to be misdiagnosed due to competing liver disease diagnoses (68% AA vs. 31% Non-AA; p< 0.002). In contrast, correctly diagnosed NASH pts were more likely to be Non-AA (64% Non-AA vs. 36% AA; p< 0.002 (Figure 1).
Discussion: In our study, almost half of the pts with NASH were misdiagnosed with NAFLD and AA patient were more likely to have a missed diagnosis of NASH. This data suggests that while the incidence of NAFLD/NASH is increasing, there remains a knowledge gap. Although guidelines for NAFLD/NASH surveillance are not well defined, proper surveillances still requires a correct non-biased initial diagnosis.

Disclosures:
Astha Saini, DO1, Anirudh R. Damughatla, DO1, Paul H. Naylor, PhD2, Milton G. Mutchnick, MD2. P2372 - Bias-Influenced Misdiagnosis of NAFLD in the African American Community, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Wayne State University School of Medicine, Detroit, MI
Introduction: Nonalcoholic fatty liver disease (NAFLD) is becoming the most common chronic liver disease in the United States. Accurate diagnosis is mandatory as advanced fibrosis (NASH) is a predictor of liver-related mortality and requires close monitoring. The African American (AA) population has a known low incidence of NAFLD. We sought to assess if there was a similar trend in our patient (pt) population. During our data analysis, we found that African American individuals were more likely to be misdiagnosed.
Methods: Using ICD-10 codes, we identified pts between 2017 and 2020 who had the diagnosis of NAFLD (K76.0) or NASH (K75.81). We defined NAFLD pts as those with significant steatosis and minimal fibrosis and NASH pts as those with significant steatosis and advanced fibrosis (F2-F4).
Results: We identified 290 pts charts which contained the ICD-10 codes for NAFLD and NASH. The charts were evaluated for accuracy of ICD-10 coding, 216 pts (75%) met the criteria for NAFLD/NASH and 74 pts had other competing liver disease (Table 1). We divided pts into those diagnosed by a gastroenterologist (GI) (n= 158) vs Non-GI (n=132), there was no difference in the misdiagnosis rate (26% vs 24%). Of the 216 pts who met criteria for either NAFLD or NASH, 39 pts were diagnosed with NAFLD but met the criteria for NASH. These underdiagnosed pts were half the total number of pts with NASH in our pt pool. In contrast, only 7 pts were incorrectly diagnosed with NASH but did not have fibrosis and thus met the criteria for NAFLD (7/46, 15%). When racial disparity was assessed, AA pts were more likely to be misdiagnosed due to competing liver disease diagnoses (68% AA vs. 31% Non-AA; p< 0.002). In contrast, correctly diagnosed NASH pts were more likely to be Non-AA (64% Non-AA vs. 36% AA; p< 0.002 (Figure 1).
Discussion: In our study, almost half of the pts with NASH were misdiagnosed with NAFLD and AA patient were more likely to have a missed diagnosis of NASH. This data suggests that while the incidence of NAFLD/NASH is increasing, there remains a knowledge gap. Although guidelines for NAFLD/NASH surveillance are not well defined, proper surveillances still requires a correct non-biased initial diagnosis.

Figure: Racial distribution for patients diagnosed correctly and incorrectly with respect to NASH vs NAFLD. AA patients were more likely to be incorrectly diagnosed with NAFLD instead of NASH as compared to Non-AA patients.
Disclosures:
Astha Saini indicated no relevant financial relationships.
Anirudh R. Damughatla indicated no relevant financial relationships.
Paul Naylor: Janssen Biotech Inc – Grant/Research Support.
Milton Mutchnick: Chronic Liver Disease Foundation – Speakers Bureau. Janssen Biotech Inc – Grant/Research Support.
Astha Saini, DO1, Anirudh R. Damughatla, DO1, Paul H. Naylor, PhD2, Milton G. Mutchnick, MD2. P2372 - Bias-Influenced Misdiagnosis of NAFLD in the African American Community, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

