Monday Poster Session
Category: Liver
P2375 - Regional Variation in Baseline Characteristics and Clinical Outcomes of Decompensated Cirrhosis With Hepatic Hydrothorax
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Mohamed Ismail, DO
Rutgers New Jersey Medical School
Newark, New Jersey
Presenting Author(s)
Mohamed Ismail, DO1, Jennifer C. Asotibe, MD1, Emmanuel Akuna, MD2, Bubu Banini, MD, PhD3
1Rutgers New Jersey Medical School, Newark, NJ; 2Einstein Healthcare Network, Philadelphia, PA; 3Yale School of Medicine, New Haven, CT
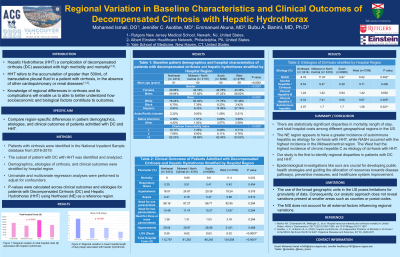
Introduction: Hepatic hydrothorax (HHT) is a complication of decompensated cirrhosis (DC) associated with high morbidity and mortality. Studying regional differences in cirrhosis and its complications allows for a better understanding of how factors such as lifestyle, environmental exposure, genetics, and healthcare disparities contribute to outcomes. To date, no studies have ascertained regional differences related to HHT across the United States (US). Here, we aimed to analyze region-specific differences in patient demographics, etiologies, and clinical outcomes of patients admitted with DC and HHT.
Methods: Patients with cirrhosis were identified in the National Inpatient Sample database from 2016-2019. The subset of those with DC with HHT was identified and analyzed. Demographic characteristics, etiologies of cirrhosis, and clinical outcomes (including length of stay [LOS] and total hospital costs) for patients with HHT were stratified by hospital region: Northeast (NE; used as reference), Midwest/North Central, South, and West. Univariate and multivariate regression analyses were performed to adjust for confounders.
Results: A total of 15,397 patients with DC and concurrent HHT were identified and analyzed. Mortality rates varied across regions, with the highest rate in the West vs. the NE (11.04% vs. 9.00%; p=0.002). The Midwest/North Central and West had mortality rates of 9.89% and 9.6%, respectively. Mean LOS for NE, Midwest/North Central, West, and South were 9.35, 8.62, 8.63 and 8.32 days, respectively. Total hospital costs were highest in the West ($134,558), followed by NE ($112,797), South ($96,245) and Midwest/North Central ($91,263). Regional differences in etiologies of DC with HHT were also noted. Non-alcoholic steatohepatitis (NASH) was more prevalent in the Midwest/North Central vs the NE (11.97 % vs. 8.78%, p=0.002), while the West had the lowest prevalence of NASH vs the NE (6.92% vs. 8.78%, p=0/002). Chronic hepatitis C was more prevalent in the West vs the NE (9.87% vs. 8.33%, p=0.005). Autoimmune hepatitis had a higher prevalence in the NE vs the West (2.07 vs. 1.26; p=0.021).
Discussion: Hospitalized patients with DC and HHT across the US shows regional variations in mortality rates, LOS, and hospital charges. The West had the highest mortality rates and hospital costs. Additionally, there were region-specific differences in etiologies of DC with HHT. Our findings of locoregional differences may play a role in the delivery of care to patients with DC and HHT.
Disclosures:
Mohamed Ismail, DO1, Jennifer C. Asotibe, MD1, Emmanuel Akuna, MD2, Bubu Banini, MD, PhD3. P2375 - Regional Variation in Baseline Characteristics and Clinical Outcomes of Decompensated Cirrhosis With Hepatic Hydrothorax, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Einstein Healthcare Network, Philadelphia, PA; 3Yale School of Medicine, New Haven, CT
Introduction: Hepatic hydrothorax (HHT) is a complication of decompensated cirrhosis (DC) associated with high morbidity and mortality. Studying regional differences in cirrhosis and its complications allows for a better understanding of how factors such as lifestyle, environmental exposure, genetics, and healthcare disparities contribute to outcomes. To date, no studies have ascertained regional differences related to HHT across the United States (US). Here, we aimed to analyze region-specific differences in patient demographics, etiologies, and clinical outcomes of patients admitted with DC and HHT.
Methods: Patients with cirrhosis were identified in the National Inpatient Sample database from 2016-2019. The subset of those with DC with HHT was identified and analyzed. Demographic characteristics, etiologies of cirrhosis, and clinical outcomes (including length of stay [LOS] and total hospital costs) for patients with HHT were stratified by hospital region: Northeast (NE; used as reference), Midwest/North Central, South, and West. Univariate and multivariate regression analyses were performed to adjust for confounders.
Results: A total of 15,397 patients with DC and concurrent HHT were identified and analyzed. Mortality rates varied across regions, with the highest rate in the West vs. the NE (11.04% vs. 9.00%; p=0.002). The Midwest/North Central and West had mortality rates of 9.89% and 9.6%, respectively. Mean LOS for NE, Midwest/North Central, West, and South were 9.35, 8.62, 8.63 and 8.32 days, respectively. Total hospital costs were highest in the West ($134,558), followed by NE ($112,797), South ($96,245) and Midwest/North Central ($91,263). Regional differences in etiologies of DC with HHT were also noted. Non-alcoholic steatohepatitis (NASH) was more prevalent in the Midwest/North Central vs the NE (11.97 % vs. 8.78%, p=0.002), while the West had the lowest prevalence of NASH vs the NE (6.92% vs. 8.78%, p=0/002). Chronic hepatitis C was more prevalent in the West vs the NE (9.87% vs. 8.33%, p=0.005). Autoimmune hepatitis had a higher prevalence in the NE vs the West (2.07 vs. 1.26; p=0.021).
Discussion: Hospitalized patients with DC and HHT across the US shows regional variations in mortality rates, LOS, and hospital charges. The West had the highest mortality rates and hospital costs. Additionally, there were region-specific differences in etiologies of DC with HHT. Our findings of locoregional differences may play a role in the delivery of care to patients with DC and HHT.
Disclosures:
Mohamed Ismail indicated no relevant financial relationships.
Jennifer C. Asotibe indicated no relevant financial relationships.
Emmanuel Akuna indicated no relevant financial relationships.
Bubu Banini indicated no relevant financial relationships.
Mohamed Ismail, DO1, Jennifer C. Asotibe, MD1, Emmanuel Akuna, MD2, Bubu Banini, MD, PhD3. P2375 - Regional Variation in Baseline Characteristics and Clinical Outcomes of Decompensated Cirrhosis With Hepatic Hydrothorax, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
