Monday Poster Session
Category: Liver
P2395 - Tobacco Use Screening and Cancer Related Outcomes in Former and Active Smokers After Liver Transplant
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- SR
Stacey Rolak, MD, MPH
Mayo Clinic
Rochester, MN
Presenting Author(s)
Stacey Rolak, MD, MPH, Kymberly Watt, MD
Mayo Clinic, Rochester, MN
Introduction: Lung and oropharyngeal cancers occur at higher rates in liver transplant recipients (LTRs) than in the general population, with smoking as a known risk factor. Our aims were to 1) identify smoking resumption rates post-liver transplant (LT) and frequency of interventions to assist with smoking cessation and 2) determine lung and oropharyngeal cancer screening practices post-LT and cancer-related outcomes.
Methods: Retrospective single center cohort study of consecutive adult liver transplant recipients from 3/1/2015-11/1/2019. We examined patients with former or current tobacco use at the time of transplant.
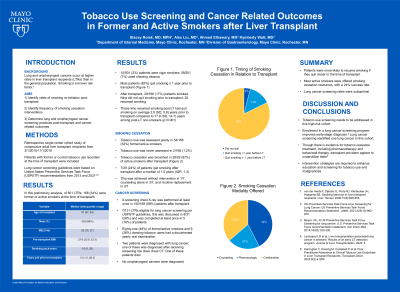
Results: Of 501 LTRs, there were 168 (34%) former or active smokers at the time of transplant (Table 1). Ten patients were cigar smokers and 35 were chewing tobacco users. Seven LTRs did not quit prior to LT (4.2%), 23/168 (13.7%) quit smoking < 1 year prior to LT, and 138/168 (82%) quit smoking ≥ 1 year prior to LT. After transplant, 29/168 (17%) resumed or continued smoking. Those who resumed smoking post-LT had quit smoking on average 2.9 (SD, 5.8) years prior to transplant compared to 17.9 (SD, 14.7) years among post-LT non-smokers (p< 0.001). Tobacco use was assessed yearly in 54/168 (32%) and was never assessed in 2 (1.2%) after transplant. Tobacco cessation was broached with 28/29 (97%) of active smokers. Counseling alone was utilized in 12, pharmacologic treatment alone in 6, and a combination of both in 10. Seven (24%) of patients quit smoking after transplant after a median of 1.5 years (IQR, 1,3); 1/7 quit without intervention, 3/7 with counseling alone, and 3/7 with nicotine replacement. Screening CXR was completed for 150/168 (89%). Of 31 LTRs eligible for lung cancer screening with low dose chest CT, this was discussed in 8 (26%) and was completed at least once in 5 (16%). Eighty-one (48%) of former/active smokers and 9 (26%) chewing tobacco users underwent yearly oropharyngeal cancer screening. Two patients were diagnosed with lung cancer; one was CT eligible, and cancer was diagnosed after receiving low dose chest CT. No oropharyngeal cancers were diagnosed.
Discussion: Patients were more likely to resume smoking if they quit closer to the time of transplant. Tobacco use screening needs to be addressed in this high risk cohort. Most active smokers were offered cessation resources with a 24% success rate. Cancer screening for high risk individuals needs improvement. Intervention strategies are required to enhance education and screening for tobacco use and malignancies.
Disclosures:
Stacey Rolak, MD, MPH, Kymberly Watt, MD. P2395 - Tobacco Use Screening and Cancer Related Outcomes in Former and Active Smokers After Liver Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Lung and oropharyngeal cancers occur at higher rates in liver transplant recipients (LTRs) than in the general population, with smoking as a known risk factor. Our aims were to 1) identify smoking resumption rates post-liver transplant (LT) and frequency of interventions to assist with smoking cessation and 2) determine lung and oropharyngeal cancer screening practices post-LT and cancer-related outcomes.
Methods: Retrospective single center cohort study of consecutive adult liver transplant recipients from 3/1/2015-11/1/2019. We examined patients with former or current tobacco use at the time of transplant.
Results: Of 501 LTRs, there were 168 (34%) former or active smokers at the time of transplant (Table 1). Ten patients were cigar smokers and 35 were chewing tobacco users. Seven LTRs did not quit prior to LT (4.2%), 23/168 (13.7%) quit smoking < 1 year prior to LT, and 138/168 (82%) quit smoking ≥ 1 year prior to LT. After transplant, 29/168 (17%) resumed or continued smoking. Those who resumed smoking post-LT had quit smoking on average 2.9 (SD, 5.8) years prior to transplant compared to 17.9 (SD, 14.7) years among post-LT non-smokers (p< 0.001). Tobacco use was assessed yearly in 54/168 (32%) and was never assessed in 2 (1.2%) after transplant. Tobacco cessation was broached with 28/29 (97%) of active smokers. Counseling alone was utilized in 12, pharmacologic treatment alone in 6, and a combination of both in 10. Seven (24%) of patients quit smoking after transplant after a median of 1.5 years (IQR, 1,3); 1/7 quit without intervention, 3/7 with counseling alone, and 3/7 with nicotine replacement. Screening CXR was completed for 150/168 (89%). Of 31 LTRs eligible for lung cancer screening with low dose chest CT, this was discussed in 8 (26%) and was completed at least once in 5 (16%). Eighty-one (48%) of former/active smokers and 9 (26%) chewing tobacco users underwent yearly oropharyngeal cancer screening. Two patients were diagnosed with lung cancer; one was CT eligible, and cancer was diagnosed after receiving low dose chest CT. No oropharyngeal cancers were diagnosed.
Discussion: Patients were more likely to resume smoking if they quit closer to the time of transplant. Tobacco use screening needs to be addressed in this high risk cohort. Most active smokers were offered cessation resources with a 24% success rate. Cancer screening for high risk individuals needs improvement. Intervention strategies are required to enhance education and screening for tobacco use and malignancies.
Disclosures:
Stacey Rolak indicated no relevant financial relationships.
Kymberly Watt indicated no relevant financial relationships.
Stacey Rolak, MD, MPH, Kymberly Watt, MD. P2395 - Tobacco Use Screening and Cancer Related Outcomes in Former and Active Smokers After Liver Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
